In The News
FLORIDA TODAY
Focus on eyes: Two-for-one: You can receive a combined cataract and glaucoma surgery
By DR. FREDERICK HO
December 28, 2021
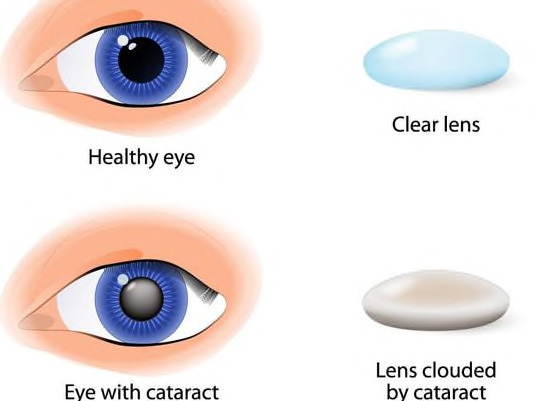
Cataract develops when the lens inside the eye becomes cloudy as we get older.
When cataracts cause visual difficulty, cataract surgery is recommended.
During the surgery, the cloudy lens is removed and then replaced with an artificial intraocular lens to regain normal vision.
Glaucoma is an eye disease of increased pressure inside the eye.
The high eye pressure damages the optic nerve, which is the nerve that sends images from the eye to the brain.
Glaucoma diminishes the vision gradually and if untreated will eventually cause permanent blindness.
The most common type of glaucoma is open angle glaucoma with high eye pressure due to resistance to fluid drainage from the eye. It is treated with medicine, laser and surgery.
Cataracts and glaucoma are the two most common eye diseases in the United States.
Both diseases are more prevalent in the older population.
Many people have both cataracts and glaucoma at the same time.
When glaucoma is not adequately controlled and the cataract makes it hard to see, your ophthalmologist may recommend combined glaucoma and cataract surgery.
The combined surgery requires one visit to the operating room so it is more convenient, lower risk and more cost effective.
The glaucoma surgery, trabeculectomy or tube shunt surgery, helps to lower the eye pressure and prevents further damage to the optic nerve.
Many patients will have less need for glaucoma medicine.
Sometimes there is a pressure rise after cataract surgery. With simultaneous glaucoma surgery, the eye pressure is stable during the post operative period.
For patients with glaucoma that are well controlled, when the cataracts are sufficiently cloudy to need surgery, they may benefit from minimally invasive glaucoma surgery, or MIGS, at the same time.
These new glaucoma procedures use the same cataract incision to enter the eye.
Most MIGS surgeries involve removing the area of resistance of eye fluid outflow or bypassing it with small stents.
The healing process is about the same as cataract surgery.
Many people will have good vision and require less or no medicine for glaucoma when the eyes heal.
The treatment of glaucoma and cataract in each patient is an individual and personalized decision.
The ophthalmologist and the patient working together will determine if cataract surgery alone, glaucoma surgery by itself or combined cataract and glaucoma surgery is the best treatment option.
Dr. Frederick Ho, the medical director of Atlantic Eye MD and Atlantic Surgery and Laser Center, is a board certified ophthalmologist. Atlantic Eye MD is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: The indirect effects on the eyes from COVID-19
By DR. FREDERICK HO
May 25, 2021
The COVID-19 pandemic started more than a year ago.
During this period of time, more than half a million Americans have lost their lives.
The Centers for Disease Control and Prevention recently updated its recommendations for mask wearing and social distancing, so continue to monitor those for the latest.
However, one thing that hasn't changed: you still should frequently wash your hands to prevent the spread of this virus, and all other illnesses.
However, in trying to keep your hands clean, you can be putting your eyes at risk.
Hand sanitizer stations and children
Hand sanitizer is a convenient substitute for soap and water.
We find free-standing hand sanitizer stations in grocery stores, gas stations, schools and workplaces.
Most of the hand sanitizer dispensers are set up so the hand sanitizer liquid is released at the waist level of an adult.
The nozzle of the dispenser is often at the eye level of younger children.
Accidental spray of hand sanitizer into the children’s eyes may happen as a result.
Hand sanitizer contains a high concentration of alcohol. Small amounts into the eye can cause burning and irritation.
Large amounts can produce corneal abrasion, a scratch on the surface of the eye or keratitis, an open sore on the cornea which is the transplant tissue in front of the eye.
Immediate rinsing of the eye with water is the first line treatment of any sanitizer liquid in the eye.
If the irritation persists, contact your ophthalmologist or visit an urgent care facility.
Ideally, a separate lower hand sanitizer can be set up for the children.
Potential damage from ultraviolet light
Many facilities follow intensive cleaning protocols including ultraviolet light and a variety of disinfecting solutions to kill the coronavirus.
Accidental exposure to ultraviolet light can cause photokeratitis, which is equivalent to sunburn to the cornea of the eye.
The ultraviolet light temporarily damages the surface of cornea.
The eyes feel light-sensitive, burning and pain. The symptoms may last hours to days depending on the duration of exposure.
The posting of signs of ultraviolet use and proper eye protection help to prevent photokeratitis.
Flee the screen and go outside
During the COVID-19 pandemic, many children are staying home and learning online.
Screen time has increased and outdoor activities have decreased.
A study of more than 100,000 school-aged children in China found a significant increase in myopic or near-sighted during 2020.
Outdoor playtime and frequent breaks from screen use can slow down the myopia progression.
Currently COVID-19 vaccines are available in all states for adults and children of a certain age.
Wide spread immunization against the coronavirus will lessen the risk of viral infection and the indirect effects on the eyes.
Dr. Frederick Ho, the medical director of Atlantic Eye MD and Atlantic Surgery and Laser Center, is a board certified ophthalmologist. Atlantic Eye MD is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Can a cataract come back after surgery?
By DR. FREDERICK HO
May 26, 2020
A frequently asked question from my patients who plan to have cataract surgery is, "will my cataract come back?"
The answer is no, but an "after cataract" may develop.
Cataract surgery is recommended when the natural lens inside the eye becomes cloudy and decreases the person’s ability to see.
The human lens has a cellophane-like outer lining called the lens capsule.
During the cataract operation, the front or anterior part of the capsule is opened to allow the removal of cloudy cataract inside the eye.
An artificial lens implant is then put inside the lens capsule in the eye and normal vision is restored with healing.
The lens capsule can thicken and become opaque after cataract surgery.
This lens capsule opacity is called "after cataract."
This can happen weeks or months after cataract operation, but more commonly occurs about one or two years after surgery.
The opaque and thickened lens capsule interferes with light transmission to the retina so the sight becomes hazy and there may be glare in bright light and halos at night.
As the "after cataract" progresses, the person notices the sight diminished as if the cataract comes back.
A YAG laser capsulotomy is a special laser treatment for "after cataract" to improve the vision.
During the procedure, a laser beam is used to create an opening in the center of the back or posterior lens capsule which lets light through.
The procedure is done outpatient and no fasting or sedation is necessary.
The laser is painless and the vision is restored quickly to how it was after the initial cataract operation.
After the laser capsulotomy, some people may experience floaters for a few days.
While the YAG laser capsulotomy is very effective, as with any laser or surgical treatments, rare complications can occur such as the pressure inside the eye rises, swelling and detachment of retina and inflammation in the eye.
When the vision changes "after cataract" surgery, it is important to contact your ophthalmologist.
A laser capsulotomy will help to improve the sight if the after cataract or capsule opacity is at fault.
Dr. Frederick Ho, the medical director of Atlantic Eye MD and Atlantic Surgery and Laser Center, is a board certified ophthalmologist. Atlantic Eye MD is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Cocaine, meth, other vices affect eyes more than you know
By DR. FREDERICK HO
April 21, 2020
An unhealthy lifestyle translates into many health problems.
Smoking, binge drinking and illicit drug use are known to cause cancer, diabetes, heart disease, lung damage, stroke and death. They can also lead to serious eye problems.
Cigarette smoking remains a major health issue despite of years of health warnings and public awareness campaigns.
Smoking has been linked to early development of macular degeneration and cataracts.
Compared to non-smokers, people who smoke a pack or more per day are two-to-three times more likely to develop macular degeneration — an aging condition in the retina, affecting the central vision.
The inhaled substances in cigarette smoke constrict the blood vessels and promote blood clot formation in the retina and optic nerves.
Partial to almost complete blindness happens when there is thrombosis, or blood clot, in the central retinal artery, which is the main artery that supplies blood, oxygen and nutrients to the retina.
Smoking increases the risk of ischemia, or stroke, in the optic nerve, which transmits the images from the eye to the brain, resulting significant permanent visual loss.
About one-in-six adult Americans binge drinks about four times a month, consuming about eight drinks each time.
There is a well-established linkage between Type 2 diabetes and excessive alcohol consumption.
The most serious ocular complications of diabetes is diabetic retinopathy. The diabetes-damaged retina develops hemorrhages and swelling, resulting in visual loss.
Alcohol abuse increases the incidence of early onset of cataracts and macular degeneration.
Methanol, or wood alcohol, in contaminated moonshine damages the optic nerve, and if untreated, the person will suffer partial to total blindness.
Ocular trauma with visual loss is too often seen with alcohol intoxication.
Illegal substance abuse is at the extreme end of vices.
It is estimated about 10 percent of adults use illegal drugs.
There are many deleterious effects to the eyes.
Intranasal cocaine use is particularly damaging and potentially leading to acute attack of angle closure glaucoma, retinal hemorrhages and optic nerve damage.
Smoking crack cocaine is associated with infection and diminished blood flow to the retina.
Methamphetamine use is known to cause infection in the cornea which is the transparent tissue in front of the eye.
Retinal inflammation is also seen in methamphetamine use.
Intravenous drug abuse introduces infection to the eyes and particles clotting the blood vessels in the retina and the optic nerve.
Many people assume their vices will get their eyes red and eyelids droopy.
In fact, they can suffer from many sight threatening complications.
Hopefully, this will motivate them to give up their vices and adopt healthy habits.
Dr. Frederick Ho, the medical director of Atlantic Eye MD and Atlantic Surgery and Laser Center, is a board certified ophthalmologist. Atlantic Eye MD is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Celebrating America's first black ophthalmologist
By DR. FREDERICK HO
February 25, 2020
David McDonogh was born into slavery on a plantation in New Orleans, Louisiana, in 1821.
His owner, John McDonogh, owner of a cotton and sugar plantation and one of the wealthiest men in the south, had a plan to free his slaves over the course of 15 years. He would allow them to work an extra day a week to gain wages that would eventually allow them to buy their freedom.
He thought the freed men and women could eventually emigrate to Liberia, a country on Africa's west coast.
John McDonogh chose to educate several of the brightest men and women so they could become leaders in Liberia, a republic in its infancy.
In 1838, David McDonogh, 19, was sent to Lafayette College in Easton, Pennsylvania.
John McDonogh appointed Pennsylvania Senator Walter Lowrie as a legal guardian for David while he was attending college.
Because David was black and a recent slave, he was forced to take classes and meals separately from the other students.
He did not complain about his treatment because John McDonogh had the power to bring him back to New Orleans in chains as a slave again.
By his junior year, David petitioned to John McDonogh for an opportunity to study medicine as part of his college education.
With reluctance, John McDonogh allowed David to become an apprentice to a local Easton physician.
Upon graduation, David expressed his wish to continue his medical education instead of emigration to Liberia. John McDonogh gave up on David and left him without any support.
Senator Lowrie intervened on David’s behalf and introduced him to Dr. John Kearney Rogers, who was a prominent New York physician and founder of New York Eye and Ear Infirmary.
David studied medicine at the College of Physicians and Surgeons (the future Columbia University Medical School) where Dr. Rogers taught.
However the president of the medical school refused to recognize David as a bona fide graduate and did not award him a diploma.
Dr. Rogers appointed Dr. David McDonogh as a staff physician at the New York Eye and Ear Infirmary, where he was well respected by fellow eye, ear, nose and throat specialists.
Dr. McDonogh attended the infirmary for more than 11 years, making him the first African-American eye physician.
When Dr. Rogers passed away in 1850, Dr. McDonogh took Kearney as his middle name in appreciation of his mentor.
In honor of Dr. McDonogh’s legacy, the National Medical Fellowships awarded the Dr. David Kearney McDonogh Scholarship in Ophthalmology/ENT to medical students in the State of New York from a Black, Afro-Latino or Native American background who has an interest in a career in ophthalmology or ear, nose and throat.
In 2018 at the Columbia University Vagelos College of Physicians and Surgeons graduation, David McDonogh was posthumously awarded the MD degree he would have received more than 170 years ago had he not been African-American.
Dr. Frederick Ho, the medical director of Atlantic Eye MD and Atlantic Surgery and Laser Center, is a board certified ophthalmologist. Atlantic Eye MD is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: How Vitamin A deficiency affects your eyes
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
June 25, 2019
Vitamin A is a fat-soluble vitamin that is stored in the liver.
It is important for normal vision, proper development and a well-functioning immune system, among others.
Vitamin A is found in many animal sources (chicken, fish, meat, and dairy products) as well as plant-based foods (carrots, kale, spinach, pumpkin, collard greens, apricots, papaya, tomatoes, mango, etc.).
An appropriate amount of vitamin A is important during pregnancy for normal development of the fetus and during breastfeeding. On the other hand, excess daily vitamin A during pregnancy can lead to birth defects.
Vitamin A deficiency is associated with lipid malabsorption as seen in medical conditions such as celiac sprue or inflammatory bowel disease, among others.
It also has been reported in patients with zinc deficiency and those exposed to cigarette smoke and chronic alcoholism.
Some of the signs and symptoms of vitamin A deficiency include infertility, poor development, dry skin, poor wound healing, dry eyes and night blindness.
Vitamin A deficiency also decreases the ability to fight infections; patients may also experience frequent or recurrent ear infections or urinary tract infections.
Patients who are suspected of having vitamin A deficiency need a complete eye exam and may require blood work to assess serum vitamin A levels.
Night blindness is one of the earliest and most common manifestations of vitamin A deficiency.
The eye exam may reveal a dry ocular surface and plaques on the conjunctiva (clear layer on top of the white sclera) near the cornea (clear layer in front of the iris / pupil). Progression of this condition can even lead to destruction of the cornea.
Vitamin A deficiency can be treated with vitamin A supplements based on the age of the individual.
It is important to have a complete eye exam if someone experiences any changes in vision or has any ocular discomfort.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Why do I need glasses to see better?
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
April 23, 2019
In most cases, when vision declines, we can use glasses or contact lenses to correct it.
Sometimes, we need to start using glasses at an early age, and some people do not require correction until later in life when presbyopia sets in and patients start to have problems with near vision.
Under normal circumstances, we are able to see clearly when the rays of light focus onto the retina (the innermost layer of the eye involved in processing light information to be sent to the brain).
When light does not focus onto the retina, then we have a refractive error.
There are several types of refractive errors that most commonly can be corrected with glasses or contact lenses like, for example, myopia (near-sightedness), hyperopia (far-sightedness), astigmatism and presbyopia.
Myopia is a condition in which the rays of light will focus in front of the retina. In this case, patients can see up close, but distance vision is blurry.
Patients with high myopia tend to have a larger than normal anterior to posterior eye length.
It is important for patients with high myopia to have a dilated exam because they have an increased risk for developing retinal detachments.
In hyperopia or far-sightedness, the rays of light will focus behind the retina, creating near vision problems. When young, hyperopic patients still have the strength within the eye to focus at distance and are able to see without glasses, but this effort may lead to eye strain and headaches.
Astigmatism is a condition in which the cornea (clear structure in front of the iris and pupil) resembles more the shape of a football instead of a round shape like a basketball.
In astigmatic eyes, the rays of light focus on different spots in front or behind the retina. If the amount of astigmatism is high, patients who are fitted for contact lenses will require special lenses to correct it.
As we age, usually after age 40, the ability of our eyes to focus on near tasks decreases. This is when people start to adjust the newspaper or restaurant menus at a distance farther than what they were used to.
This is the time when patients develop presbyopia and the need for reading glasses.
Presbyopia is a normal aging process in which there is progressive inability to clearly focus on nearby objects due to a hardening of the crystalline lens (clear structure inside the eye that later on becomes cloudy and is called cataract).
Patients with presbyopia usually start to complain of problems reading small print letters, especially in low light conditions. They also develop the need of having to adjust the distance of their reading material.
As we grow older, the crystalline lens becomes cloudy, and this cloudiness is what we call cataract.
Cataract surgery is advised once the cataract have progressed to the point that glasses or contact lenses do not improve the vision and patients have difficulty performing activities of daily living like driving, watching TV or reading.
If you are having trouble with your vision and you notice that you don’t see as well as you used to, you should have an eye exam and discuss with your eye doctor the best options that will help you improve your sight.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: I have a growth on my eye?
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
August 21, 2018
The sclera is the white part of the eye, which is covered by a clear layer called conjunctiva.
Chronic exposure to the ultraviolet rays from the sun can cause changes in these layers, and two of those changes are called pinguecula and pterygium. These two are more prevalent in tropical climates.
A pinguecula is a benign yellow/whitish deposit on the conjunctiva that does not involve the cornea (clear layer in front of the colored part of the eye).
A pinguecula usually does not cause any symptoms; however, it occasionally can become inflamed. It grows slowly and usually artificial tears help minimize any discomfort. A pinguecula rarely requires surgery.
A pterygium is a pinkish, benign growth that extends from the sclera onto the cornea. It usually presents on the nasal portion, but occasionally it can occur laterally.
A pterygium usually grows very slowly over the years, and if left untreated it can cross the pupil, thus permanently affecting vision.
If the growth remains stable, the treatment involves conservative management with lubrication, decreased sun exposure by wearing sunglasses with ultraviolet protection and repeated measurements of the pterygium are taken to assess for any growth.
If the pterygium continues to grow or if it is approaching the visual axis, it is recommended to excise it and place a graft to cover the lesion.
Once the pterygium is removed, there will be scars on the cornea, and that is why it is important to remove it before it approaches the visual axis because this can permanently decrease the patient’s vision.
Recurrences can occur; therefore, it is extremely important to prevent sun damage to the eyes to avoid recurrences.
Since both, pingueculae and pterygia are elevations on the ocular surface, they can potentially become dry and irritated. Thus, it is advisable to lubricate the eyes with artificial tears to prevent this.
When pingueculae or pterygia are irritated, patients complain of foreign body sensation, red eyes, tearing, and itching among others.
In some cases, topical steroids can help improve the irritation.
Contact lens intolerance can be also attributed to enlarged or irritated pingueculae or pterygia.
It is important to wear sunglasses with ultraviolet protection to prevent their continued growth. Patients should follow up with their ophthalmologists to address any changes noticed on their eyes and any potential growth that can decrease or impair their vision.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: How the eyes help monitor Wilson’s Disease
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
July 24, 2018
Wilson’s disease is a rare genetic disorder in which copper accumulates in the body. It usually affects the liver and the brain, but can also involve the kidneys, the heart and the eyes.
Symptoms are usually expressed between the ages of 5 and 35.
When the liver is affected patients start to complain of fatigue and they have increased tendencies for bleeding and in some severe cases even confusion.
Cirrhosis of the liver can also occur due to chronic hepatitis.
The diagnosis comprises liver function tests, coagulation studies, ceruloplasmin (copper-carrying protein in blood) levels (usually low in Wilson’s disease), serum and urine copper levels, brain imaging if neurological problems are present and a liver biopsy, which is the ideal test to diagnose the disease.
About 50 percent of patients with Wilson’s disease have neurological or psychiatric symptoms.
Initially patients develop mild cognitive problems. Patients may become clumsy and even have behavioral changes. These patients can develop symptoms similar to Parkinson’s disease in which patients have rigidity and slow movements.
Patients with Wilson’s disease can also have migraine headaches, tremors and even seizures. Some patients with Wilson’s disease develop depression, anxiety and psychosis usually in addition to the previously mentioned symptoms.
The ocular problems are rare; however, patients with Wilson disease can have a ring of brown/red/green pigmentation in the periphery of the cornea (clear layer in front of the pupil) called Kayser-Fleisher ring, which represents cooper deposits.
In early development of the Kayser-Fleisher ring, the ophthalmologist will use a specialized lens to visualize the angle structures - drainage system of the eye and determine if patients with Wilson’s disease are developing this ring, which normally at first appears superiorly and eventually forms a complete ring.
Patients can also develop cataracts from copper deposition. If the cataract affects the vision, patients may benefit from cataract surgery.
The treatment involves a diet low in copper-containing products. Some medications help increase the removal of copper from the body, while others prevent its absorption from the diet. In some cases, liver transplant is a consideration for treatment. This is a progressive disease and without treatment it can even be fatal.
Patients with Wilson’s disease are frequently examined by ophthalmologists to determine if they have Kayser-Fleisher ring, and to check if the patient is responding to treatment.
If the treatment is successful, the deposits on the cornea will resolve, although some corneal changes may remain. Therefore, this pigmented ring can be used to monitor the patient’s response to treatment.
Recurrence of the Kayser-Fleisher ring formation can suggest non-compliance or no response to the medication. Patients that have Wilson’s disease should be closely followed by their primary doctors and should have regular eye exams.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: High blood pressure can affect your eyes
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
April 24, 2018
High blood pressure, or hypertension, is a medical condition in which blood pressure remains elevated.
Smoking, being overweight, excess salt consumption and alcohol intake increase the risk of developing high blood pressure.
Hypertension is usually asymptomatic; however, chronic elevated blood pressure increases the risk of developing coronary artery disease, kidney disease, heart failure, stroke, peripheral vascular disease, memory problems and can even lead to vision problems.
Some people with severe high blood pressure levels may experience headaches and shortness of breath. However, hypertension usually gives no symptoms.
Chronically elevated blood pressure can lead to hypertensive retinopathy, a condition in which the eyes show stiffened micro-vasculature bleeding and micro-infarcts of the retina (innermost layer inside the eye), and even swelling of the optic nerve (nerve that transmits visual information from the eyes to the brain).
While chronic vascular changes from high blood pressure do not usually cause any symptoms, some patients may present with eye pain, headaches or decreased vision.
Changes in the vessels inside the eye increase the risk of retinal artery or vein occlusion, which can lead to permanent loss of vision. The treatment for hypertensive retinopathy is management of systemic blood pressure.
Most people with high blood pressure have no identifiable cause, and hypertension tends to develop gradually over the years. This type of high blood pressure is called primary or essential hypertension.
On the other hand, some people develop secondary hypertension, which is due to an underlying condition like for example kidney problems, sleep apnea, thyroid problems, adrenal gland tumors, illegal drug use, alcohol abuse and even some prescribed medications.
There are several types of medications that can be used alone or in combination to help control elevated blood pressure. Make sure that you follow with your primary care physician to address any health issues, and have a yearly eye exam if you have elevated blood pressure.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Sickle cell disease and your eyes
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
March 20, 2018
Sickle cell disease is an inherited form of anemia in which the red blood cells become rigid, sticky and do not carry adequate amounts of oxygen to the body.
The abnormal red blood cells can get trapped in the small vessels, thus blocking or slowing down blood flow and oxygenation to the tissues. Sickle cell anemia is most often seen in people of African descent.
People with sickle cell anemia may experience recurrent episodes of severe abdominal, chest or musculoskeletal pain that may require hospitalization.
Some patients with sickle cell anemia may develop painful swelling of hands and feet due to decreased blood flow. If the spleen is affected by the disease, patients become more prone to infections. Sickle cell crisis can be triggered by dehydration, temperature changes, stress and high altitude.
Sickle cell disease is diagnosed by analyzing blood samples for abnormal hemoglobin (blood protein involved in transport of oxygen). In the United States, newborns are usually screened for sickle cell at the hospital.
People with sickle cell anemia usually have no ocular symptoms; however, when the disease affects the eyes, patients may have decreased vision, flashes and floaters.
Sickle cell disease can affect the retina (innermost layer inside the eye) causing the formation of new vessels that may lead to bleeding inside the eye, which can lead to loss of vision.
Retinal detachments also have been observed in patients with sickle cell disease affecting the eye.
If the patient has neovascularization (formation of new vessels) of the retina with bleeding into the vitreous (gel inside the eye), ophthalmologists treat the area with laser and/or inject medications into the eye to help regress those new vessels and prevent future bleeding.
Trauma to the eye on a patient with sickle cell anemia can lead to bleeding into the anterior portion of the eye and elevated intraocular pressure, which needs to be controlled rapidly in order to prevent permanent loss of vision.
A patient with sickle cell disease needs annual eye exams including dilation of pupils; however, if the disease involves the retina, closer follow ups are needed to prevent and manage a possible loss of vision depending on the severity of the disease.
Some serious complications of sickle cell anemia include high blood pressure, organ damage, loss of vision and the life-threatening acute chest syndrome in which the patient experiences chest pain, fever and difficulty breathing.
There is no cure for sickle cell anemia, but there are treatments to prevent problems associated with it, to relieve pain and to manage any ocular problems. If you have sickle cell disease or trait, follow your primary care physician closely and have at least a yearly eye exam.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Long-term Plaquenil intake can affect your vision
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
February 20, 2018
Plaquenil, or hydroxychloroquine, is an anti-malaria medication that is commonly used to treat autoimmune disorders like lupus or rheumatoid arthritis.
During World War II, it was found that antimalarial drugs helped improve fatigue, fever and skin rashes as well as joint and muscle pain, which are common symptoms in lupus.
Years later, doctors started to prescribe antimalarials drugs to their patients diagnosed with lupus.
Plaquenil is taken by mouth with food or milk to prevent stomach problems. When taking this medication, some patients may experience upset stomach, nausea, loss of appetite, headaches or dizziness.
Sometimes, taking high doses or long-term treatment of Plaquenil can lead to vision problems. Chronic treatment has been associated with damage to the retina (inner most layer or the eye involved in processing light stimulus).
Plaquenil toxicity can cause pigmentary changes in the macula (area where central vision is processed) and visual field defects leading to vision loss.
For this reason, patients who are taking Plaquenil should have at least one eye exam a year to screen for toxicity.
Once retinal toxicity is found, the medication needs to be stopped; however, in some cases, vision loss progresses even after discontinuation of Plaquenil.
Some patients with toxicity affecting the macula may experience a delay in the recovery time following exposure to bright lights. Patients may notice a decrease in vision at distance and near, develop sensitivity to light or detect blacked out areas in their central field of view.
At a screening for retinal toxicity due to Plaquenil intake, the ophthalmologist will do a complete eye exam including dilation of the pupils to look at the inner layers of the eye.
Images of the retina will be taken and a specialized visual field test for Plaquenil toxicity screening will be performed.
Some risk factors for Plaquenil toxicity include short height, obesity, liver disease, kidney disease and macular disease.
If you are taking Plaquenil, you should have an eye exam, even if you have no vision problems.
In most cases, toxicity can be detected by the ophthalmologist before it is noticeable by the patient.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: What is Bell’s palsy?
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
November 28, 2017
Bell’s palsy is a neurological condition in which there is a dysfunction of the nerve (cranial nerve VII or facial nerve) that controls the muscles of the face and manifests as a paralysis or weakness of one side of the face.
Patients with Bell’s palsy present with a one-sided droopy face and asymmetric smile. They may also have altered taste and increased sensitivity to sound.
Bell’s palsy also affects the eyelid muscles and patients are not able to completely close one eye; thus, leading to dry eye symptoms that if untreated can lead to corneal damage and even blindness.
To prevent these eye problems, it is recommended frequent lubrication with artificial tear drops, gel or ointment, and patching of the eye in the affected side. In more severe cases, it may be necessary to suture part of the upper and lower eyelids together to decrease the exposure of the eye in order to decrease the effects of the cornea drying out.
The cause of Bell’s palsy remains unknown. However, it is thought that it may be due to a viral infection leading to swelling of the nerve. Nevertheless, this occurs more commonly in patients with diabetes than in otherwise the healthy population.
Bell’s palsy affects men and women equally; though, reports indicate that it is more likely to occur in pregnant women (especially during the third trimester) than non-pregnant women.
Bell’s palsy usually improves on its own; however, treatment includes corticosteroids within a few days after onset. Steroids can help recover muscle function.
Some people may benefit from physical therapy to help maintain the muscle tone of the affected facial muscles. Some patients may have nerve re-growth that goes to the wrong place, thus causing, for example, eyelid closure when attempting to smile or vice versa. In cases in which Bell’s palsy does not improve, surgery can be an option; this procedure is called “Smile Reconstruction.” As the name implies, the surgery attempts to restore the patient’s smile.
Not all cases of facial weakness represent Bell’s palsy; facial paralysis can also be associated with brain tumors, stroke or Lyme disease.
People that experience muscle weakness or paralysis should immediately be seen by their primary care physician or at the emergency department to determine the proper course of action.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
HOMETOWN NEWS
2017
Dr. Frederick Ho was presented with Readers' Choice Award in Best Eye Care for 2017 and for 5 years in a row.
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Cancer and the eyelids
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
October 24, 2017
Cancer can affect any part of the body, and skin cancer is more prevalent than any other type of cancer in the United States.
It is estimated that about 45 percent of Americans older than 65 years of age will develop basal cell carcinoma or squamous cell carcinoma, which are two of the most common types of skin cancer, and they can also occur on the eyelids.
Patients with skin cancer to the eyelids may present with swelling of the eyelid, chronic eyelid infections, discoloration of the eyelid, ulceration of the skin of the eyelid, distortion of normal eyelid anatomy, loss of eyelashes or whitening of eyelashes over the lesion among other signs and symptoms.
Basal cell carcinoma and squamous cell carcinoma are two of the most common types of cancer that affect the eyelids.
Basal cell carcinoma usually affects the lower eyelid but it can occur anywhere around the eye, and it is generally seen in middle-aged and older individuals. This type of cancer rarely metastasizes, but can be locally invasive, thus destroying the normal anatomy of the eyelids and face.
Squamous cell carcinoma presents similarly to basal cell carcinoma, but regional metastasis can occur where surrounding nervous tissue and orbit invasion can be observed.
Sebaceous cell carcinoma is a rare malignancy of the glands that are located in the eyelids. It presents as a yellowish discoloration of the eyelids, and it can mimic chronic or recurrent styes.
Sebaceous cell carcinoma is more common in women older than 60 years of age and it involves the upper lid more often than the lower lid. A full thickness wide excisional biopsy is required to confirm the diagnosis, to assess the extent of tumor the invasion, and to attempt to remove the entire lesion at once.
If a lesion is suspicious for cancer, the growth or abnormal area is biopsied, and if the diagnosis of cancer is confirmed, the lesion is excised completely.
Not all eyelid lesions are cancer. There are benign tumors on the eyelids like for example papillomatous warts, which look like skin tags, and are caused by a papilloma virus infection.
This occurs more commonly in middle-aged or elderly people. These warts can be surgically removed if cosmetically unappealing or causing any discomfort.
Dermoid cyst is another type of benign lesion that can present on the eyelids. This cyst presents at birth and becomes evident when it starts to enlarge.
This lesion is round, firm and usually involves the lateral portion of the upper eyelid. It can also extend into the orbit; therefore, imaging is performed to visualize the extend of the lesion. Surgical excision is curative.
While there are malignant and pre-malignant skin changes, most eyelid lesions tend to be benign growths. However, they need to be examined and monitored.
It is well accepted by the medical and scientific community that skin cancer correlates with exposure to ultraviolet rays from the sun. As a result, everyone should protect themselves from the ultraviolet rays by applying sunblock lotions, wearing sunglasses with ultraviolet protection and wearing hats whenever spending time outdoors.
To this point, there are even SPF (Sun protection factor) protective clothing and hats to better protect ourselves from the sun rays.
If you are concerned or notice any changes in your eyelids or your skin, consult your primary care physician, ophthalmologist or dermatologist about it.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
CONSUMERS' RESEARCH COUNCIL OF AMERICA
2017
Dr. Frederick Ho has met all requirements and has been selected as one of AMERICA'S TOP OPHTHALMOLOGISTS
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Lyme disease can affect eyes
By DR. JUAN CARLOS DE RIVERO VACCARI AND DR. FREDERICK HO
September 26, 2017
Lyme disease is caused by a type of bacteria (Borrelia) that are transmitted to people through the bite of an infected blacklegged tick.
The symptoms can start from as early as a few days after exposure up to months or even years after the initial contact.
The chances of getting Lyme disease depend on the type of tick and how long the tick was attached to the skin. Generally, the tick has to be attached to the skin longer than 36 hours to spread the bacteria.
The early symptoms of Lyme disease include headaches, fever, fatigue, muscle pain, joint pain, chills and swollen lymph nodes.
A high number of infected people will develop a bull’s eye type of skin rash (called erythema migrans), which occurs at the site of the tick bite. This rash can grow in size, and usually does not cause any itching nor pain.
If untreated, patients can develop facial nerve palsy (weakness/paralysis of face muscles) and meningitis (inflammation of the brain that causes severe headaches and stiff neck).
If not treated appropriately, some people may develop eye problems, abnormal heart rhythm, impairment of muscle function, joint pain, and memory loss.
Some of the eye problems that occur when patients are infected with Lyme disease include conjunctivitis (red eye), decreased vision, ocular pain, as well as inflammation of the iris (colored part of the eye), cornea (clear layer in front of the colored iris), retina (inner most layer of the eye) or optic nerve (nerve that connects the eye to the brain).
The diagnosis is based on clinical signs and symptoms and a history of exposure to ticks. Blood work may also be ordered to confirm Lyme disease, but this can be negative in the early stages. Lyme disease is treated with antibiotics, and the earlier the treatment is started the better the recovery.
To prevent getting bitten by ticks when hiking or camping in the woods, make sure you wear a long-sleeved shirt, long pants, socks and boots. You should use tick repellents, and if possible, wear clothing that contains DEET (Diethyltoluamide).
Since the previous winter was relatively mild, the number of the population of ticks is expected to increase this year, and therefore increase the number of people that may get bitten and potentially develop Lyme disease.
It is important to check your skin if you have been camping or hiking in areas prone for ticks. If you have been bitten by a tick, remove it with a pair of tweezers as soon as possible, and make sure no parts of the tick remain on your skin.
Once, the tick has been removed, clean the area with alcohol or soap and water.
Most infections occur in endemic areas in the United States such as the northeast, mid-Atlantic, north central states and west coast.
So, it is important to be careful when traveling or living in tick-prone areas, and make sure to go see your primary care physician if you have been bitten by a tick.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
HEALTH FIRST
2017
Dr. Frederick Ho, congratulations on 30 years of service at Holmes Regional Medical Center.
Return to Top of Page
Viera Voice
Personal touch is Atlantic Eye MD’s proven approach
By Julie Sturgeon
August 31, 2017
 Dr. Frederick Ho has proudly served patients in Brevard for the past 30 years, and he has no plans to stop anytime soon.
Dr. Frederick Ho has proudly served patients in Brevard for the past 30 years, and he has no plans to stop anytime soon.
During his tenure as an ophthalmologist, Ho has provided eye care to thousands of Brevard residents. His practice, Atlantic Eye MD, focuses on providing compassionate vision service.
“We emphasize individual, personalized eye care. I’ve been here 30 years, people know me and they know my staff,” Ho said. “I like to help people see better. It’s my passion in life.”
The eyes are extremely susceptible to injury and disease, and Ho has treated patients for all kinds of eye afflictions, including eye injuries, double vision, partial blindness, swelling and cataracts.
Eye emergencies are not uncommon, and Ho has made more than one late night trip to the emergency room. Especially rewarding for Ho has been treating generations of family members during the past 30 years.
“I have treated grandparents, parents, children, four generations; I’ve see the progression of disease as my patients age,” Ho said. “So, we have taken care of many family members.”
Last year, Ho welcomed ophthalmologist Juan Carlos de Rivero Vaccari, M.D., Ph.D. to his practice. Ho speaks highly of Vaccari, who completed his residency just prior to joining Atlantic Eye MD. Vaccari, a Board Eligible Ophthalmologist, specializes in cataract surgery, laser surgery, diabetic eye disease, macular degeneration and glaucoma management, among other ocular conditions.
“Dr. Vaccari is establishing himself,” Ho said. “Patients have started to seek him out because they have a good experience here, and want to come back.”
Vaccari is enthusiastic about serving patients at Atlantic Eye MD. He shares a deep desire to connect on a personal level with patients while educating them about the importance of eye protection.
“The most common complaint I hear from my patients coming from other practices, is that everything is very rushed, nobody knows them,” Vaccari said. “That’s one reason why they like coming here.”
Ho agrees, saying, “It’s not a huge bureaucracy here, when you call to make an appointment you will talk to someone instead of getting a phone tree. When you come in, you see the same doctors and staff rather than having to interact with new (staff) every time.”
A community-minded physician, Ho offers his expertise to the Brevard Health Alliance, the Lupus Foundation and the association for the Advancement of the Blind. Notably, Ho once instructed doctors while performing eye surgery in China on a jet equipped with an operating room for Project ORBIS, an organization focused on blindness prevention.
Vaccari will carry on this tradition of service.
Both physicians are active outside of work and very family oriented. Ho has four daughters, which keep him busy attending their activities, while Vaccari and his wife enjoy traveling and visiting museums in their spare time.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: How solar eclipses can affect eyes
By DR. FREDERICK HO AND DR. JUAN CARLOS DE RIVERO VACCARI
July 25, 2017
On Aug. 21, 2017, those living in or visiting the states along a stretch from Oregon to South Carolina will be able to see a total solar eclipse (other areas in North America will get a partial solar eclipse).
A solar eclipse occurs when the moon blocks a part of the sun from our view. During a total solar eclipse, the moon covers the entire sun, and daylight becomes twilight. Then, as the celestial bodies continue to move, the outer portion of the sun will glow like a halo around the moon.
Gazing directly at the sun (sun-gazing or eclipse viewing) without any special solar filters can lead to damages to the retina (nervous tissue inside the eye that sends visual information to the brain via the optic nerve).
This damage is called solar retinopathy, in which there is usually damage to the fovea, the portion of the retina involved on our finest central vision.
As a result, the vision can be affected. In some cases, it takes several months for visual acuity to improve following an onset of solar retinopathy; however, some people may have permanent damage and even develop more blind spots on their field of view.
Patients with solar retinopathy usually complain of decreased vision, development of blind spots, visual disturbances (for example, wavy lines instead of being straight) and even headaches.
Regular sunglasses, even if there are very dark, will not protect the eyes from staring at the sun. To observe the sun there is only one safe way — with the use of special solar filters.
If the solar filters are scratched or damaged, they may not protect you from the solar rays. When looking at a solar eclipse, the only safe time to look at it without any protective gear is during a total solar eclipse; however, as the sun rays begin to appear, you need to place your solar filters on.
Also, do not look at the sun through cameras or telescopes that don’t have solar filters. Solar eclipses are wonderful events to observe, but only with the right gear.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Why do my eyes burn?
By DR. FREDERICK HO AND DR. JUAN CARLOS DE RIVERO VACCARI
May 23, 2017
Why do your eyes burn? It could be dry eyes.
The tears are made of water, oil and mucus, which are produced by different glands on the eye surface and the eyelids.
Any deficiency in the production or the quality of any of these components will lead to dry eyes.
Blinking spreads the tears all over the eye surface, and the tears normally drain through the canals that are located near the nose on the eyelids; the tears then flow through the nasolacrimal ducts into the back of the nose, which also connected to the mouth. This is why sometimes, when we place drops on our eyes, we can taste the medication.
The function of the tear film is to lubricate the ocular surface, protect the eye from infections, wash away foreign particles and provide nourishment to the ocular surface. For clear vision to occur, it is important to have a smooth surface that is created by the tear film. Any abnormality in the tear film may lead to blurry vision.
Eye burning is a common complaint when the eyes are dry. Furthermore, having dry eyes is a common problem that can occur at any age but usually manifests or worsens as we age.
Some of the signs and symptoms of dry eyes also include blurry vision that improves after blinking, grittiness, scratchy feeling, redness, light sensitivity, tearing, foreign body sensation as if sand or an eye lash is stuck on the eye, difficulty wearing contact lenses and even pain.
Dry eye is a multifactorial disease; it can be due to a physiological response in which there is less production of tears or problems with the quality of the tear film.
Women are more prone to dry eyes than men due to hormonal changes.
Dry eyes can be due to inflammation in the anterior ocular surface, environmental issues, evaporation of the tears, or systemic conditions like Sjogren’s syndrome or rheumatoid arthritis.
Vitamin A deficiency can lead to dry eyes among other problems.
Skin disorders like acne rosacea can also affect the ocular surface and cause dry eyes.
Smoking and exposure to wind, smoke or dry environments can cause evaporation of the tear film, causing or exacerbating dry eye symptoms.
Likewise, when we are focusing on a task, like watching TV, reading, working on the computer or driving, we tend to blink less, which causes tear evaporation and can cause dry eye symptoms.
Eye dryness could also occur as a side effect of certain medications like antihistamines, decongestants, acne medications or birth control pills among others.
Laser refractive surgery, like LASIK, can cause or worsen dry eyes, although the symptoms are for the most part temporary.
The routine treatment of dry eyes involves using over-the-counter artificial tears of different viscosities ranging from watery to gel-like type tears.
There are also ointments that can be used to lubricate the eyes, but these are mainly used at bed time since they will blur the vision but keep the eyes moist throughout the night while sleeping.
Sometimes, patients feel that when they wake up they have sticky, irritated eyes with foreign body sensation and burning and even get crusty eyelids. This could be due to the eye being not fully closed while sleeping. Some people sleep with the eyes a little open and this creates an opening where air will dry the eyes.
In these cases, it is particularly important to apply artificial tear-lubricants in ointment form before going to sleep.
Another case in which the ointment can help while sleeping is in those patients that use a CPAP/sleep apnea machine to help with breathing while sleeping.
These machines tend to blow air onto the face which can dry the eyes.
Additionally, silicone punctum plugs can be implanted in the ducts that drain the tears into the nose to aid prolong the time that the tears are in contact with the ocular surface, thus ameliorating the symptoms of dry eyes.
Reports suggest that increasing oral consumption of omega-3 fatty acids/fish oil can help in the management of dry eyes.
In some cases, eyelid disease such as blepharitis or acne rosacea can contribute and worsen dry eyes. It is also advisable to do warm compresses and use lid scrubs or cleaning the eyelashes with baby shampoo and water to help decrease the inflammation along the eyelid margin and help with the production of the components of the tear film.
It is important to wear sun glasses to protect the eyes from the drying effects of the wind and the sun. If the dry eye symptoms are moderate to severe, wraparound sunglasses are more appropriate.
Also, try to increase the humidity levels in your home or workplace so that the eyes don’t dry that easily.
Currently, there are two prescription drugs for the treatment of dry eyes: Restasis and Xiidra.
Restasis is an immune suppressant eye drop that helps control the inflammatory response that contributes to dry eyes.
Xiidra is another prescription eye drop that helps block the secretion of inflammatory molecules that cause dry eyes.
You should talk to your eye doctor if you have any signs and symptoms of dry eyes that are not ameliorated by the use of artificial tears because you may benefit from punctum plugs or medications such as Restasis or Xiidra.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on eyes: Why do I see black spots?
By DR. FREDERICK HO AND DR. JUAN CARLOS DE RIVERO VACCARI
April 25, 2017
Inside the eye, between the crystalline lens (where cataracts form) and the retina (the innermost layer of the eye) there is a clear gel, called the vitreous body, or vitreous humor, which is made of water, salts, sugars, proteins and collagen.
The vitreous humor is present since birth, and as we age, this gel-like substance becomes watery and forms condensations.
As rays of light enter the eye and strike those condensations, people start seeing black spots. These black spots are shadows originating from these condensations.
This is what occurs when patients start to describe that they see flies or mosquitoes that are not real and that they are the only ones who see them.
Similarly, patients may also see squiggly lines, half circles or full circles floating in the air. In addition, patients might complain that the spots move whenever they move their eyes.
These condensations that might be perceived as spots or lines are called floaters, and they will be more noticeable when the patient is in a bright environment, looking at a white wall or white piece of paper, watching television or working on the computer. If the floaters are located more centrally, they will be perceived more often than as if they were located in the far periphery of the vitreous humor.
As we age, the vitreous humor tends to separate from the retina. It is in that time when patients will notice a large floater and may even see flashes of light.
As the vitreous humor separates from the retina, it stimulates the retina leading to notice a flash of light. In some cases, small tears or holes may be created in the retina during the process of the vitreous detaching from the retina.
Any tear or hole can lead to accumulation of fluid underneath the retina causing a retinal detachment. Retinal tears or holes can be easily treated by performing a laser to create a barrier, thus decreasing the risk of retinal detachment.
Floaters are fairly common, but there are a few things that we need to be aware of. When someone develops multiple new floaters combined with flashes of light and a black curtain is dropping, this is a sign of retinal detachment. This is an emergency and requires a dilated fundus exam by an ophthalmologist.
A retinal detachment repair is a more laborious surgery, in which the ophthalmologist will remove the vitreous humor and use either gas or oil to attempt to reattach the retina. Laser may be used to seal any tears or holes, and to anchor the periphery of the retina.
The retina contains multiple cells that will process light and send information to the brain through the optic nerve so that we can see images.
Therefore, any damage to the retina can be detrimental to our sight, and considering that floaters are fairly common, everyone should be aware of the signs of retinal detachment such as increased in number of floaters, flashing lights, decreased vision or a black curtain dropping through our field of view.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Surgery should be done by surgeons
By Dr. Frederick HO
March 28, 2017
Most physicians and surgeons focus on sciences during their four years of college education and then immerse in a very challenging medical school study for four more years. Those who become surgeons participate in three to five years of residency during which they learn their clinical and surgical skills under direct supervision of experienced surgeons.
In the current Florida Legislature session, HB 1037 would allow optometrists, who are not medical doctors or surgeons, to perform laser and scalpel surgery after completing an unspecified course and examination. To become ophthalmologists or eye surgeons, the medical school graduates participate in three or more years of residency and fellowship training. They spend years of learning and practicing eye laser and surgery to become proficient and safe eye surgeons.
Oklahoma is one of the few states where optometrists are allowed to perform laser surgery. Experts from the University of Michigan recently conducted a study that compared surgical outcomes of laser surgeries performed by ophthalmologists in Oklahoma to those performed by optometrists. The results of that study was startling. It shows the frequency of repeated surgeries by optometrists was more than double the frequency of repeat surgeries by ophthalmologists. Adverse surgical events, repeat surgeries and surgical complications only harm patients, they drive up healthcare costs by requiring additional surgical procedures and forcing patients out of the workplace for longer periods of time.
In a debacle in a Veterans Administration Hospital in California, optometrists practiced beyond their scope, which resulted in many of our veterans being blinded.
Medical doctors or physicians who are trained in non-surgical specialties, such as internal medicine or pediatrics do not perform surgery because they recognize the complexity and challenges of surgery.
In the book “Outliers,” author Malcom Gladwell presents The 10,000-Hour Rule. Researchers find 10,000 hours of practice is required to have expertise in complex skills in anything. There is no shortcut for hard work or substitute through legislature to master complex eye laser or surgery.
HB 1037 which allows optometrists who do not have formal medical education or years of surgical training to perform eye laser or surgery after completing a course and an examination, is harmful to the health of all Floridians. This dangerous legislature is bad public policy and a disservice to the citizens of Florida.
Frederick Ho, MD, FACS is a board certified ophthalmologist and a fellow of American College of Surgeons who has practiced in Brevard County for 30 years.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: Transient vision loss
By Dr. Juan Carlos De Rivero Vaccari and Dr. Frederick HO
February 21, 2017
Individuals can experience a transient loss of vision for a variety of reasons; some serious, some minor. Depending on the circumstances that launched the vision loss, the condition can last for a few seconds, several minutes or an hour.
Causes of transient vision loss include a swollen optic nerve, decreased blood flow to the eye (amaurosis fugax), migraine headaches (classic or ocular), inflamed arteries (arteritis) and strokes.
Swelling of the optic nerve occurs when intracranial pressure (pressure inside the skull) becomes elevated, causing temporary vision loss with posture changes or eye movements. The loss typically lasts for only a few seconds.
Once diagnosed with a swollen optic nerve, an ophthalmologist seeks the reason. The answer typically results from brain imaging and an analysis of cerebrospinal fluid from a lumbar puncture. A swollen optic nerve could also be the unintended effect of a medication. Tetracycline antibiotics, contraceptives and drugs containing high doses of vitamin A derivatives increase intracranial pressure that, in turn, could initiate swelling in the optic nerve.
Temporary vision loss is also attributed to vascular problems; decreased blood flow to the eye due to vasospasms, low blood pressure, carotid artery disease, heart disease, blood clots or blood disorders.
Amaurosis fugax is a condition of a monocular vision loss (or reduction) lasting from a few minutes to more than thirty. Brief, recurrent episodes of amaurosis fugax often suggest an impending central retina artery occlusion that could result in permanent vision damage.
Bilateral vision loss frequently indicates vertebrobasilar artery insufficiency. A patient with this condition may also have vertigo, poor control of body movements, numbness or even paralysis. These are serious symptoms requiring immediate medical attention.
Another source of transient vision loss are migraines; with and without headaches (ocular). Either condition can result in vision loss ranging from a few minutes to over an hour. These patients usually have a personal or family history of migraines.
The visual deficit episode usually begins with blurry vision or a zig-zagging light or a visual field defect preceding the headache. Migraines are more prevalent in younger people, declining after age 40. Because new migraine onset after age 50 is uncommon, ophthalmologists proceed to rule out secondary causes such as vascular events, intracranial hemorrhages, infarcts or masses.
In certain conditions, inflamed arteries swell causing their interior circumferences to shrink resulting in restricted blood flow; this is named giant cell arteritis or temporal arteritis. Symptoms include headache, scalp tenderness (particularly around the temples), jaw pain and cramping of jaw muscles or the tongue when chewing. Vision loss generally occurs in one eye but can also develop in the other eye if the inflammation goes untreated.
A diagnosis of giant cell arteritis is confirmed with blood evaluation and (possibly) a biopsy of a temporal artery. This condition is immediately treated with high dose oral steroids to prevent irreversible blindness. If the signs and symptoms are highly suggestive of giant cell arteritis, a negative biopsy does not necessarily rule out the disease. In such cases, patients are prescribed oral steroids for several months.
The degree and duration of visual loss associated with a stroke is dependent upon where the ischemic event occurs; in the eye or in the brain. Ophthalmic strokes particularly affect the retina and the optic nerve. Blood clots, hemorrhages or severe low blood pressure can permanently damage vision. It is important for everyone to have routine exams to evaluate any systemic issues and ensure blood pressure, cholesterol and glucose levels (among others) are in range. As previously mentioned, cardiovascular problems other than strokes can adversely affect the eyes.
Episodes of transient vision loss, regardless of how short-lived or lacking in accompanying symptoms, should be evaluated by your ophthalmologist to ensure any permanent damage is prevented.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: Types of implants for cataract surgery
By Dr. Juan Carlos De Rivero Vaccari and Dr. Frederick HO
January 24, 2017
 Inside the eye, we have a lens, known as the crystalline lens. This is a clear structure when we are born but it continues to produce cells as we grow older. This is part of the normal process of aging.
Inside the eye, we have a lens, known as the crystalline lens. This is a clear structure when we are born but it continues to produce cells as we grow older. This is part of the normal process of aging.
As a result of aging, the crystalline lens form opacifications, which are called cataracts. As cataracts progress, the vision decreases, colors decrease in intensity and patients start complaining of glare and difficulty seeing while driving, especially at night. In addition, patients describe troubles performing other common activities such as reading. Cataracts can be surgically removed once it reaches a point in which vision is compromised.
Cataract surgery involves removal of the cataract (opacified cyrtalline lens) and insertion of an intraocular lens implant to help restore vision. Most patients will get an implant that is set for distance and they will need to use glasses for near tasks such as reading.
Nowadays, we have more options when it comes to what to select as an intraocular lens implant after cataract extraction. Depending on the corneal surface and the patient’s needs, we now can select toric intraocular lenses, monofocal lenses and multifocal intraocular lenses.
Astigmatism is a condition in which the cornea (clear structure in front of the pupil and colored part of the eye) loosely resembles the shape of a football instead of being spherical like a basketball. Astigmatism will cause rays of light to fall at different points in front or behind the retina, thus leading to poor vision. Prior to cataract extraction, the ophthalmologist will do several measurements and if the patient has astigmatism, he or she could benefit from toric intraocular lenses. These lenses will correct the astigmatism minimizing the chances of requiring glasses for distance.
We also have some options to correct both distance and near at the time of cataract surgery such as monofocal vision, multifocals and accommodating intraocular lenses. Monofocal vision involves one eye corrected for distance while the other eye is corrected for reading vision.
Patients that opt for this usually have used contact lenses with monofocal correction in the past, so they are used to this modality. If a patient has never worn monofocal contact lens correction, but desires monofocal vision after cataract surgery, then the patient will need a trial period using soft contact lenses with a monofocal correction in which one eye is fit for distance and the other one for near. If successful, then this option can be considered for the intraocular lens implants during cataract surgery.
Furthermore, we can choose multifocal lenses in which one lens provides distance and reading vision. These types of lenses provide great vision; however, after surgery a few patients describe issues with glare and halos depending on the type of lens utilized. Some of these issues resolve over time.
Multifocal lenses are not used in patients that have problems in the macula (area where our central fine vision is located) such as macular degeneration due to an increase risk in diminishing the quality of vision when compared to other type of implants.
Nowadays, we have more options than in the past when it comes to intraocular lens placement during cataract surgery. It is important that the patient is aware and is told about all the possible intraocular lens options including risks and benefits prior to undergoing cataract surgery to provide the best option that matches the patient’s vision requirements.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
SPACE COAST LIVING HEALTH
Comprehensive and Coordinated Eye Care for Brevard Residents
Winter, 2017

Click to Read in the Online Digital Edition.
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: How the Zika virus damages eyes
By Dr. Frederick HO and Dr. Juan Carlos De Rivero Vaccari
December 27, 2016
Vision begins in the eye with light patterns on the retina. The images produced by those patterns are perceived in the brain. Their link is the optic nerve.
Diseases and infections in the brain can present in the eyes, especially the retina. Microcephaly, which is an underdeveloped brain inside an abnormally small head, is one of them. Microcephaly has recently been a world news story because it is directly associated with the Zika virus.
Infected mosquitoes transmit the Zika virus when they bite humans. When those mosquitoes bite pregnant women, the mothers can transmit the virus to their fetus.
Serious eye abnormalities are associated with microcephaly in the newborn, ranging from undeveloped retinal vessels to damages to developing retinal vessels including hemorrhaging. Vision loss can result from malnourished retinal tissue. Microcephaly is also associated with lesions that obstruct vision by decreasing peripheral vision and producing blind spots. Depending upon severity and treatability, this too can cause vision loss.
Unfortunately, in many cases, the mothers of infants infected with the Zika virus did not realize they had acquired it. Symptoms associated with Zika are also associated with common, minor maladies such as fever, rash and joint pain. Ocular symptoms are less common. They include inflammation of the iris and the conjunctiva in addition to insufficient blood flow to and within the retina. Individually, none of these conditions point to Zika, but combined they do. Those patients should be queried about recent travels outside the continental U.S. and history of mosquito bites if the live in or have traveled to Florida.
Because of the direct link between microcephaly and vision disorders, it is recommended that all microcephalitic newborns receive an ophthalmic examination. However, medical researchers discovered that not all newborns infected with Zika are microcephalitic, so the ophthalmic examination recommendation has been expanded to include all infants whose mothers were diagnosed with the Zika virus and not just microcephalitic newborns.
Another reason for the expanded recommendation is that an eye abnormality may be present in Zika infants that does not occur in those with microcephaly. This birth defect is called torpedo maculopathy; a type of lesion acquiring its name from its shape and location within the eye. This lesion presents in the macula — the center of the retina where high definition light patterns occur. The macula produces neuronal signals from these patterns that travel the optic nerve to the cerebral cortex where the image is perceived. A torpedo-shaped lesion on the macula significantly interferes with this process. The size and number of torpedo lesions determines the severity of vision loss.
Medical researchers have also discovered that some children infected with Zika are experiencing late onset of the ocular disorders associated with microcephaly; “born healthy” but developing vision problems years later. As a result, the ophthalmic examination recommendations have been amended again to include periodic evaluations throughout a Zika patients’ childhood to prevent undiagnosed ocular disorders.
The Centers for Disease Control provides a list of foreign travel destinations where the Zika virus is prevalent. The U.S. territories of Puerto Rico, the Virgin Islands and Samoa have captured Zika infected mosquitos. Florida is the only continental state to do so.
Mosquito control is currently the best prevention against Zika. Zika virus testing is recommended for pregnant patients with symptoms compatible with Zika virus disease.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: What is macular degeneration?
By Dr. Juan Carlos De Rivero Vaccari and Dr. Frederick HO
November 22, 2016
In the innermost part of the eye we find the retina, and the portion of the retina that is involved in capturing our fine central vision is called macula.
In age-related macular degeneration (AMD), there is a loss of central vision while the peripheral vision remains intact (this is opposite to glaucoma, a disease in which the peripheral vision is damaged prior to affecting the central vision, thus leading to a tunnel vision).
Patients with macular degeneration usually complain of blurry vision, distorted images, central blind spots, straight lines that appear wavy, difficulty recognizing faces, trouble driving and problems reading. However, at the beginning of the disease, patients may not have any symptoms.
There are two types of age-related macular degeneration: Dry AMD and Wet AMD. Approximately 85 to 90 percent of people affected with macular degeneration will have the dry type.
In the early stages of macular degeneration, fatty protein particles deposit in the retina, which eventually lead to abnormal changes in central vision.
In wet AMD, anomalous blood vessels grow below the retina, which leads to leakage of fluid and even blood.
As of today, there is no cure for macular degeneration, but there are treatments that help prevent the advancement of this condition. Scientific research has shown that taking a combination of antioxidant minerals and vitamin supplements known as AREDS 2 can prevent the progression of the disease in patients with intermediate and advanced AMD.
For patients with wet AMD, we now have intraocular injections like Avastin, Lucentis or Eylea that help with the issues associated with this type of AMD by decreasing the growth of the abnormal blood vessels and slowing the leakage. The treatment with intraocular injections is initially monthly, but the interval between injections can be later on extended once the disease is under control.
AMD typically occurs in older individuals. It is also more common in caucasians and it has a genetic component, which means that it runs in families. Some other risk factors include cigarette smoking, light iris color, high cholesterol, high blood pressure, cardiovascular disease and hyperopia (farsightedness).
There also is a juvenile form of macular degeneration called Stargardt disease, which has an onset during the first two decades of life. Young patients with Stargardt disease present with decreased vision, and in early stages of the disease process, the vision is worse than the clinical findings.
For patients diagnosed with macular degeneration it is important to quit smoking and to avoid areas where others are smoking because smoking can accelerate the progression of the disease.
AMD is diagnosed by performing a complete eye exam that includes dilation of the pupils to observe the retina, the deepest layer of the eye. If you have symptoms of AMD or if you have a family member with AMD, you should have your eyes examined by an eye doctor.
It is important to remember that the earlier that macular degeneration is diagnosed and treated, the better the chances of preserving central vision.
Dr. Ho and Dr. Vaccari are ophthalmologists at Atlantic Eye MD, specializing in cataract surgery, multifocal lens implants, laser surgery, diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders.
The Atlantic Eye MD office is located at 8040 N. Wickham Road in Melbourne. To make an appointment please call (321) 757-7272. To learn more about the personalized eye care of Dr. Ho and Dr. Vaccari, visit AtlanticEyeMD.com
Return to Top of Page
SPACE COAST LIVING HEALTH
Health Care Professionals - Juan Carlos De Rivero Vaccari
Fall, 2016
 Dr. Juan Carlos de Rivero Vaccari found his calling in ophthalmology as a teenager. “I always liked the eye when I was a little kid. I was 15 when my uncle was diagnosed with a corneal condition which eventually required a corneal transplant,” de Rivero Vaccari said. “I even remember where I was standing in the house when I found out. That’s when I thought to myself, ‘I’m going to become an ophthalmologist and try to help people.’“
Dr. Juan Carlos de Rivero Vaccari found his calling in ophthalmology as a teenager. “I always liked the eye when I was a little kid. I was 15 when my uncle was diagnosed with a corneal condition which eventually required a corneal transplant,” de Rivero Vaccari said. “I even remember where I was standing in the house when I found out. That’s when I thought to myself, ‘I’m going to become an ophthalmologist and try to help people.’“
De Rivero Vaccari continues, “A lot of people go into medicine not knowing how they intend to specialize. I liked other specialties during my different rotations in medical school, but nothing compared to ophthalmology for me. The procedures and technology are always changing and these new discoveries make it so exciting.” He received his bachelor of science degree in biology from Florida
International University, graduated summa cum laude and became a member of the Phi Beta Kappa Honor Society while earning other multiple awards.
After graduation, he moved to New Orleans, Louisiana, to pursue a Ph.D. in neuroscience from the Department of Cell Biology and Anatomy at Louisiana State University Health Sciences Center. While focusing on cell death mechanisms in the brain, he received the Chancellor’s Award. Subsequently, Dr. de Rivero Vaccari completed a postdoctoral fellowship at the LSUHSC Neuroscience Center of Excellence, where he investigated neuroprotective and neurodegenerative pathways in the retina.
Purposely shifting gears back to clinical training, he then obtained his medical degree from Louisiana State University School of Medicine in New Orleans. During his tenure, Dr. de Rivero Vaccari was awarded the Golden Probe Award and was elected as a junior into the prestigious Alpha Omega Alpha Honor
Society. He completed his intern/preliminary year at the Department of Internal Medicine at
Ochsner Medical Center, and his residency in ophthalmology at Louisiana State University
School of Medicine/Ochsner Medical Center.
Dr. de Rivero Vaccari is currently a board eligible ophthalmologist licensed in the state of Florida. He is a published author with several scientific and clinical publications in respected journals. He specializes in cataract surgery, laser surgery, diabetic eye disease, macular degeneration and glaucoma management, among other ocular conditions.
Atlantic Eye offers patients comprehensive, concentrated, coordinated eye care – from diagnosis through sophisticated surgery. Continuity of care is a key component of successful treatments, as well as an essential element of Atlantic Eye’s personalized eye care.
Return to Top of Page
FLORIDA TODAY
Prostate meds can cause eye surgery problems | By Dr. Frederick Ho
October 25, 2016
When you swallow a pill, the medicine travels throughout your body interacting with all your organs and tissues; some more than others depending upon the chemicals consumed. That’s why potential side effect warnings are lengthy.
Ophthalmologists recently discovered that a popularly-prescribed drug to treat Benign Prostatic Hyperplasia (BPH) adversely affects the functionality of the eye’s iris and pupil.
This unforeseen side effect causes complications during cataract surgery in a significant number of patients. This irregularity is referred to as Intraoperative Floppy Iris Syndrome (IFIS).
The drug is Flomax (Tamsulosin), an alpha blocker. Another BPH medication with Tamsulosin as an active ingredient is Jalyn. Other BPH medications with differing active ingredients also adversely affect the iris and pupil but to a lesser degree; Dutasteride (Avodart) and Finasteride (Proscar) for example.
It’s not just BPH medications that can cause IFIS. Tissue relaxing drugs are prescribed for bladder disorders as well as hypertension. These drugs are classified as inhibitors rather than blockers. Their effect on the iris can be problematic during cataract surgery but much less so than Tamsulosin.
Commonly prescribed inhibitors include Alfuzosin (Uroxatral), Silodosin (Rapaflo), Terazosin (Hytrin) and Doxazosin (Cardura). Even saw palmetto, an herbal alternative that inhibits prostate enlargement, produces a mild form of IFIS.
The iris is the colored part of the eye. Centered is the pupil; a dark hole opening that continually changes its size in response to the amount of light required for optimal vision. The muscle that controls pupil dilation is in the iris tissue.
The active ingredients in alpha-blockers and inhibitors adversely affect the pupil’s ability to enlarge to its maximum circumference and sustain that size. Under most circumstances, this isn’t a problem.
However, because cataracts, the clouded lenses, are located directly behind the iris, the pupil must be fully dilated during cataract surgery. The pupillary dilation must be maintained from cataract removal through insertion of a new intraocular lens. Drugs that interfere with the pupil’s enlargement muscle in the iris can cause serious surgical complications if the eye surgeon is unaware that their patient is taking or, just as important, has ever taken Tamsulosin (Flomax or Jalyn), Dutasteride (Avodart), Finasteride (Proscar), Alfuzosin (Uroxatral), Silodosin (Rapaflo), Terazosin (Hytrin) or Doxazosin (Cardura).
Even residue of these medications can be problematic, so discontinuing them prior to cataract surgery is not an option.
Fortunately, ophthalmologists have developed operative procedures and tools to fully enlarge the pupil as well as prevent iris muscle prolapse (IFIS). When your eye surgeon is informed about any use of alpha-blockers or inhibitors, complication risk is significantly reduced.
Another option is to not initiate (non-emergency) alpha-blocker or inhibitor medications until after cataract surgery. If that’s not a viable option, speak with your prescribing physician about treating your condition with a medication demonstrated to produce a minimal rather than a high IFIS risk factor. Some urologists, cardiologists and primary care physicians may not know these drugs increase the risk of cataract surgery complications.
On a positive note, individuals who have already had cataract surgery need not be concerned with any ophthalmic side effects associated with alpha-blockers and other tissue relaxing medications.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
HOMETOWN NEWS
October, 2016
Dr. Frederick Ho was presented with Readers' Choice Award in Best Eye Care for 2016 and for 4 years in a row.
Return to Top of Page
FLORIDA TODAY
Health Pro: Ophthalmologist had eye on his field at young age | By GEORGE WHITE
August 9, 2016
 Dr. Juan Carlos de Rivero Vaccari can trace the exact moment he chose his specialty dealing with care, treatment and surgery on the eye, also known as ophthalmologist.
Dr. Juan Carlos de Rivero Vaccari can trace the exact moment he chose his specialty dealing with care, treatment and surgery on the eye, also known as ophthalmologist.
But, unlike most specialists, he first went the extra step of getting a related academic Ph.D. in Neuroscience so he could contribute to innovation during his medical career.
“I always liked the eye when I was a little kid. I was 15 when my mother’s brother got diagnosed with a condition with the cornea which would eventually require a corneal transplant,” he said. “I even remember where I was standing in the house when I found out. That’s when I said, ‘I’m going to become an ophthalmologist and try to help people.’“
A lot people when they go into medicine don’t know what they want to do. I liked the other specialties during the different rotations in medical school but the way I felt about them was nothing compared to ophthalmology for me. ... Pretty much my entire life has been dedicated to the eye. Things are always changing and that’s what makes it so exciting with the new discoveries.”
De Rivero Vaccari talked about his specialty and medical career, which started with him obtaining a related Ph.D. in Neuroscience with research studying the retina.
-
QUESTION: Even when you were in the Ph.D. program, did you always expect to go into medicine as a career and become a doctor?
de Rivero Vaccari: I did it to give me more overall knowledge so I could also contribute, not only from a clinical aspect but from a research aspect. When I did my post-doctoral fellowship I was studying neuroprotective mechanisms in the retina. That helped me a lot during residency in ophthalmology and I’m always doing collaborations on research.
-
Q: How timely is your specialty choice with the expected increase in business with the aging of the Baby Boomer generation, and did that figure into your career decision?
de Rivero Vaccari: As people age we are all going to need an ophthalmologist, so there will be many more patients, but the aging of the Baby Boomers did not fit into my decision. Even if a lot of people didn’t need an ophthalmologist, I would still be an ophthalmologist. Even if I didn’t make any money I would still be an ophthalmologist.
-
Q: What are some of the recent innovations in your field?
de Rivero Vaccari: the new intraocular lenses used in cataract surgery are helping people see better. Cataract surgeries at first were just to help people see. Now we can correct astigmatism and other conditions. And now a lot of lasers are coming out.
-
Q: Are the innovations in your specialty driven by new surgical procedures or are they driven by the use of new tools like lasers?
de Rivero Vaccari: I think in ophthalmology it is a little of both. It’s not just the materials. It’s also the equipment and the understanding.
-
Q: Of the innovations that have occurred over the past few years, which has made the biggest impact on patient outcomes?
de Rivero Vaccari: I think cataract surgeries nowadays are amazing. Patients have satisfaction immediately. I’ve had patients crying right afterward that they could see my face now.
-
Q: Do you do injections for macular degeneration and how do they help?
de Rivero Vaccari: There are a lot of diabetics and we treat a lot of patients with really bad diabetes. We used to inject the back of the eye a lot to prevent swelling on the back of the eye. Now it’s a great thing. Now we have injectable for wet macular degeneration. Now we have more options to inject in the eye and help the patient.
-
Q: Which is easier to treat, wet or dry?
de Rivero Vaccari: With the dry there is really nothing. You give them vitamins for prevention. With the wet in the past we did not have many options but now we have injections that help us. It doesn’t cure it but it can help keep it from advancing.
-
Q: What is on the horizon in your field?
de Rivero Vaccari: Cataract surgery will make everything perfect: 20/20. In the future I think we will use a lot of lasers to make and correct all the imperfections in the cornea and try to make everybody see 20/20.
-
Q: What area of your specialty would you most like to see progress made?
de Rivero Vaccari: There are still people who are blind from glaucoma and other retinal diseases. If we can find a way to regenerate the retina and make those people see again. If I had a magic wand I would do that: regenerate the retina so they could see again.
-
Q: What is your favorite part of your job?
de Rivero Vaccari: Whenever a patient comes to me with a problem and I’m able to help them. They are just so grateful.
-
Q: What is a frustrating or difficult part of your job?
de Rivero Vaccari: Dealing with insurance. It’s a lot of paperwork. I never imagined when I went into medicine that I would spend so many hours on paperwork.
Juan Carlos de Rivero Vaccari, Ophthalmologist
Hometown: Lima, Peru, moved to Chalmette Louisiana after high school
Family: Wife, Claudia Foronda
Hobbies: Swimming, travel, visiting museums and cultural events, watching and playing sports
Education: Associate’s Degree from Nunez Community College, Chalmette, Louisiana; Associate’s Degree in vision care, Miami Dade Community College; Bachelor of Science degree in Biology from the Florida International University, Miami; Ph.D. in Neuroscience from LSU Health Sciences Center, New Orleans; M.D. degree from the LSU School of Medicine in New Orleans. He completed his Internship in internal medicine Ophthalmology at Ochsner Medical Center, New Orleans; Residency in Ophthalmology at the LSU School of Medicine/Ochsner Medical Center, New Orleans.
Contact: Atlantic Eye MD, 8040 N. Wickham Rd., Melbourne (321) 757-7272
Return to Top of Page
SPACE COAST LIVING HEALTH
Health Care Professionals
Summer, 2016
 Dr. Frederick Ho is a board certified ophthalmologist specializing in cataract surgery, multifocal lens implants, laser surgery,
diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders. He is also recognized for his expertise in pediatric ophthalmology and strabismus surgery.
Dr. Frederick Ho is a board certified ophthalmologist specializing in cataract surgery, multifocal lens implants, laser surgery,
diabetic eye disease, glaucoma and macular degeneration as well as the full spectrum of vision disorders. He is also recognized for his expertise in pediatric ophthalmology and strabismus surgery.
Dr. Ho has been named a Top Doctor in the U.S. by Consumer’s Guide to Top Doctors and a Top Ophthalmologist by the Consumer’s Research Council of America. He is a Fellow of the American College of Surgeons and the American Academy of Ophthalmology.
An honors graduate of the California Institute of Technology, Dr. Ho earned his medical degree from Washington University, St. Louis. His ophthalmology residency was completed at Barnes Hospital and Washington University Medical Center. He was awarded a Pediatric Ophthalmology Fellowship by Children’s Hospital in Washington, D.C.
Dr. Ho and his professional staff feel very privileged their patients and medical colleagues trust them with complex surgery, accurate diagnoses and comprehensive, continuing eye care since 1987. During his years of practice in Brevard County, Dr. Ho has performed thousands of cataract surgeries and laser procedures as well as examined and treated over 30,000 patients. No two patients’ conditions have been identical. Each person is unique; an observation that inspired Dr. Ho’s credo of “Personalized Eye Care.”
An ambulatory surgery center under the directorship of Dr. Ho is adjacent to his examination and treatment complex. With state-of-the-art ophthalmic equipment, patients receive treatment for cataracts, glaucoma, diabetic retinopathy, strabismus and eyelid surgery.
“We offer patients comprehensive, concentrated, coordinated eye care — from diagnosis through sophisticated surgery if necessary,” stated Dr. Ho. “Continuity of care is a key component of successful treatments as well as an essential element of our personalized eye care.”
Dr. Ho’s “Personalized Eye Care” credo is also reflected in the friendly conversation and proficiency every patient enjoys with his experienced office staff.
A wall in Dr. Ho’s waiting area is covered with note cards of appreciation written by patients. Interior hallways feature artworks created by other thankful patients. These gifts of gratitude define “Excellence in Ophthalmology” from a patient’s perspective — as they see it.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
SENIOR LIFE
Lifestyle changes can fight crippling effects of glaucoma | By Dr. Frederick Ho
March 30, 2016
Glaucoma is a sight-threatening disease affecting the optic nerve, the direct connection between each eye and the brain. As the optic nerve deteriorates, so does vision.
In its early stages, glaucoma causes areas of blind spots in one’s peripheral vision. If untreated, blindness eventually occurs. Even with treatment, optic nerve damage can only be stopped, not reversed. Ophthalmologists have made remarkable progress in treating and controlling glaucoma but have yet to discover a cure.
Glaucoma is the second most common cause of blindness in the U.S. and is the leading cause of blindness among African Americans with elderly people being most at risk. Regardless of age or racial heritage, the most significant risk factor for developing glaucoma is high pressure inside the eye, specifically an intraocular pressure of 21mm of mercury or higher.
Other risk factors include a family history of glaucoma, near-sightedness or far-sightedness, eye injury, low blood pressure, diabetes, sleep apnea and migraines.
Glaucoma is treated in two ways; medicinally with eye drops and surgically with lasers and intraocular valve and shunt insertions.
Medical researchers have recently identified several lifestyle behaviors that positively or adversely affect the severity of a patient’s glaucoma. Beyond complying with eye drop directions, here’s what glaucoma patients can do to mitigate its development and progression:
-
Moderate exercise — Physically fit individuals have lower intraocular pressure than inactive people. Both aerobic and dynamic resistance exercises lower eye pressure. Somewhat surprisingly, in the opposite direction, is yoga. Although recommended for its relaxation benefits, certain head down yoga positions increase intraocular pressure and must be avoided.
-
Good nutrition — Optimal eye health depends on optimum ocular tissue nutrition. One’s diet determines the quality of those nutrients. Carrots, leafy green vegetables and fruits are particularly helpful to glaucoma patients, as are foods rich in omega 3 and 6 oils. In addition, Ginkgo biloba has a positive effect on ocular blood flow and improves visual function. Vitamin and mineral supplements have not shown any impact on glaucoma; even ones recommended for macular degeneration.
- Alcohol, sodas — Alcohol, in modest amounts, reduces intraocular pressure through the relaxation effect. While caffeine in coffee, tea and soda serve as a constricting agent that can increase pressure in the eye as well as throughout the body’s vascular network, a little tea or coffee is fine for glaucoma patients. However, too much caffeine at a time or during the course of a day are both detrimental.
- Tobacco use — Cigarette smokers have an increased risk of developing glaucoma. Tobacco consumption also interferes with treatment success.
- Sleep apnea — Sleep apnea is a chronic condition that interrupts breathing during sleep. In obstructive sleep apnea, the airway becomes blocked, causing breathing to stop for up to two minutes. This condition has been linked to an increased risk of glaucoma development and progression.
- Other factors — Playing high resistance wind instruments like trumpets, French horns, oboes and bassoons can elevate intraocular pressure and worsen glaucoma. Neckwear tied too tight can have similar damaging effects, especially if worn in a stressful environment.
The good news is that knowledge of these proactive and counter-productive lifestyle factors, if you make the right choices, can significantly reduce the development and progression of glaucoma-related vision loss until ophthalmologists can announce a cure.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
HOMETOWN NEWS
October, 2015
Dr. Frederick Ho has been awarded The Hometown News Readers' Choice in Eye Care for 2015 and for 3 years in a row.
Return to Top of Page
FLORIDA TODAY
Space Flight Affects Astronauts' Vision | By Dr. Frederick Ho
September 24, 2015
Astronauts have long told stories about their eyes being thrust to the back of their heads as they accelerate into the wild blue yonder. Once they achieve orbit, their eyes return to normal.
Or do they?
According to NASA, of the 48 astronauts who spent more than 90 days on International Space Station missions, 33 experienced near and distance vision problems. Those refractive changes resolved (with rare exceptions) upon return to Earth. Within that group, 22 were visually impaired. Of the 22, one-third experienced optic disc edema.
NASA’s deep-space, long-term travel plans, such as its Mission to Mars, could be jeopardized by space induced vision loss.As a result, NASA launched a two-year ocular study during a Soyuz mission to the International Space Station in March of this year.
Micro-gravity is the presumed culprit. Zero gravity causes objects to elevate including organs, tissues and body fluids. Flotation alters the position of an astronaut’s internal anatomy as well as the volume of fluids, especially the cerebrospinal fluid in the head. More importantly, blood and intracranial fluids have no anatomical outflow mechanism other than gravity. Blood flow out of the head through the jugular vein can be inhibited. Extra cerebrospinal fluid accumulating inside the skull elevates intracranial pressure that, in turn, flattens the back of a spherical eyeball resulting in blurred vision at various distances. Increased intracranial pressure bulges the optic nerves and discs, causing some astronauts to experience mild, transient, decreased peripheral vision. They do not, however, demonstrate any permanent visual field or visual acuity loss after returning to Earth.
NASA’s Mission to Mars is targeted to launch near the year 2030. The roundtrip journey will take up to 950 days prompting serious concerns regarding progressive visual loss expected to affect astronauts.
Searching for a remedy, NASA’s ophthalmic partners have invented Balance Goggles. The name refers to the eyewear’s ability to produce a balance between intracranial and intraocular pressures. Worn during sleep, Balance Goggles create a sealed, artificial environment around an astronaut’s eyes. This nightly normalization of intracranial and intraocular pressures prevents the onset of blurry vision by preventing the buildup of abnormal pressures over time.
Blurry vision is also being addressed through multi-focal-point lenses as well as glasses with interchangeable lenses to accommodate an astronaut’s fluctuating optic prescription strengths throughout their day caused by anatomical changes attributed to prolonged time in space.
NASA has an impressive history of space flight inventions that are now commonly used by Earthlings. These two developments are no exception.
Elevated intraocular pressure is the predominant cause of glaucoma. Recent research points to a significant relationship between irregular intraocular pressure and abnormal pressures elsewhere in the body; most notably cerebrospinal. By normalizing these pressures, Balance Goggles could minimize, if not eliminate, the regressive vision loss experienced by glaucoma patients – without medication.
In diabetic patients, fluctuating blood sugar levels cause periods of blurry vision. Interchangeable lenses of varying prescription strengths engineered for astronauts would improve the quality of life for millions of diabetics.
NASA’s focus on eyesight could make ophthalmology the next big beneficiary of the space program.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Lifestyle Behaviors Can Increase Risk of Glaucoma | By Dr. Frederick Ho
July 23, 2015
Glaucoma is a sight-threatening disease affecting the optic nerve – the direct connection between each eye and the brain. As the optic nerves deteriorate, so does vision. In its early stages, glaucoma causes areas of blind spots in one’s peripheral vision. If untreated, blindness eventually occurs. Even with treatment, optic nerve damage can only be stopped; not reversed. Ophthalmologists have made remarkable progress in treating and controlling glaucoma but have yet to discover a cure.
Glaucoma is the second most common cause of blindness in the U.S. and is the leading cause of blindness among African Americans. Elderly people are most at risk. Regardless of age or racial heritage, the most significant risk factor for developing glaucoma is high pressure inside the eye; specifically,an intraocular pressure of 21mm of mercury or higher. Other risk factors include a family history of glaucoma, near sightedness or far sightedness, eye injury, low blood pressure, diabetes, sleep apnea and migraine.
Glaucoma is treated in two ways; medicinally with eye drops and surgically with lasersand intraocular valve and shunt insertions.
Medical researchers have recently identified several lifestyle behaviors that positively or adversely affect the severity of a patient’s glaucoma. Beyond complying with eye drop directions, here’s what glaucoma patients can do to mitigate its development and progression.
The most important behaviors relate to activities. Physically fit individuals have lower intraocular pressure than inactive people. Both aerobic and dynamic resistance exercises lower eye pressure. Somewhat surprisingly, in the opposite direction, is yoga. Although recommended for its relaxation benefits, certain head-down yoga positions increase intraocular pressure and must be avoided.
Optimal eye health depends on optimum ocular tissue nutrition. One’s diet determines the quality of those nutrients. Carrots, leafy green vegetables and fruits are particularly helpful to glaucoma patients as are foods rich in omega 3 and 6 oils. Ginkgo biloba has positive effect on ocular blood flow and improves visual function. Vitamin and mineral supplements have not shown any impact on glaucoma; even ones recommended for macular degeneration.
Alcohol, in modest amounts, reduces intraocular pressure – the relaxation effect. Although caffeine in coffee, tea and sodais a constricting agent that can increase pressure in the eye as well as throughout the body’s vascular network, a little tea or coffee is fine for glaucoma patients. Too much caffeine at a time or over the course of a day, however, are both detrimental.
Cigarette smokers have an increased risk of developing glaucoma. Tobacco consumption also interferes with treatment success.
Sleep apnea is a chronic condition that interrupts breathing during sleep. In obstructive sleep apnea, the airway becomes blocked, causing breathing to stop for up to two minutes. This condition has been linked to an increased risk of glaucoma development and progression.
Playing high resistance wind instruments like trumpets, French horns, oboes and bassoons can elevate intraocular pressure and worsen glaucoma.
Neckwear tied too tight can have comparable damaging effects, especially if worn in a stressful environment.
Knowledge of these proactive and counter-productive lifestyle factors can significantly reduce the development and progression of glaucoma related vision loss until ophthalmologists announce a cure.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Multiple Sclerosis Affects Vision | By Dr. Frederick Ho
June 25, 2015
Multiple sclerosis (MS) is a disease of the central nervous system. Onset relates to the body’s natural defense mechanism, the immune system, erroneously attacking the nerves in our body; specifically, the membrane sheaths called myelin. In addition to protecting nerves the way plastic coating protects the bare electric wires, myelin accelerates the movement of nerve impulse. If a myelin nerve sheath is damaged, the transmission of nerve impulses becomes inefficient; stopping completely in severe cases. This process is known as demyelination which is the underlying cause of MS.
Patients with MS frequently have visual symptoms. The ophthalmologist is often the first physician consulted. Behind the eye is the optic nerve which connects the eye to the brain. It sends images from the eye to the brain so we can see. The optic nerve is one of the most prominent nerves affected by MS. This condition is referred to as optic neuritis.
When optic nerves become inflamed with demyelination, pain frequently follows as do vision abnormalities including blurry images, flashings, loss of color vision, depth perception problems and dark spots centered in visual fields. Vision loss may occur, though, usually, in only one eye at a time. Fortunately, except in rare cases, normal vision returns when the inflammation subsides. The exceptions usually involve color and diminished depth perception.
Optic neuritis is frequently the first manifestation of MS. Half of all individuals diagnosed with MS initially complained about a vision problem. Up to 75% of female patients and 35% of male patients diagnosed with optic neuritis ultimately develop multiple sclerosis. Typically, patients initially diagnosed with optic neuritis are young adults aged 20-45. The condition appears to affect Caucasians more commonly than it does other races. Women are affected twice as often as men. Medical researchers attribute these differences to genes that makes individuals more susceptible to develop optic neuritis.
Double vision is a frequent symptom of MS. Demyelination in the brain can affect its ability to coordinate eye movements. Damage from MS causes paralysis of nerves that control individual eye muscles. Jerky or dancing eye movement, nystagmus, is often observed in MS patients. Patients with eye movement problems from MS typically complain of double vision, blurry vision or objects jumping.
A gradual recovery of vision with time is characteristic of optic neuritis patients, although permanent residual deficits in color vision and contrast and brightness sensitivity are common. Visual function begins to improve one week to several weeks after onset, even without treatment. Steroids do little to affect the ultimate visual acuity in patients with optic neuritis. Specific guidelines for steroid use in treatments of optic neuritis associated with MS have been established through a large clinical trial. Double vision is treated using prisms or an eye patch.
Although there is no proven cure for MS, we have recently seen tremendous advances in MS treatment. Locally, we are fortunate to have many experienced neurologists available to consult on MS patients.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Education level, electrics use increase risk for myopia | By Dr. Frederick Ho
September 18, 2014
An estimated 40% of Americans experience some degree of myopia - the medical term for nearsightedness. Myopic vision usually occurs because the eyeball is abnormally long or the cornea is too steep.
Both circumstances cause the precise focal points of light rays to be in front of the retina instead of directly upon it. Myopic individuals see close objects just fine but distant objects are blurry.
Fortunately, myopia is easily corrected. Most people choose to wear glasses or contact lenses that redirect the light rays onto the retina producing clear images of distant objects.
Some people opt for refractive surgery such as LASIK to correct their nearsightedness. During LASIK, the laser light reduces the steepness of the corneal curvature. The reshaped cornea allows a distant image to correctly fall on the retina improving their faraway vision.
Although corrected, myopic individuals are more likely to experience serious eye disorders than people who do not have refractive abnormalities. They have an above average risk of developing glaucoma and cataracts.
An elongated myopic eyeball is more susceptible to retina tear development that can initiate retinal detachment, resulting visual loss. A detached retina is surgically repairable if detected early. It is important for individuals with myopia to have regular eye examinations so changes in the retina that may lead to retina tears or retinal detachment can be discovered.
Myopia has traditionally been regarded as an inherited condition, usually discovered between the ages of 8 and 12. It may become worse during the rapid growth teenage years.
Medical researchers have recently reported a remarkable relationship between myopia in adults and length of education - a connection more significant than genetics. The more years spent in school, the more likely one is to need glasses.
This need increases annually. A recent German study found that over 50 percent of college graduates have myopia compared to a third of those whose schooling ended with high school. Drop-outs have the fewest myopic patients – a reported 25 percent.
Scientists attribute this to time spent indoors, reading and staring at computer and smartphone screens as opposed to spending time outdoors focusing on stationary and moving objects at a distance.
The outdoor factor is important because recent research in China has demonstrated the risk of children and adolescents developing myopia can be significantly reduced by increasing time outdoors.
Ophthalmologists attribute this connection to the effect of sunlight on the rate of eye growth in children. Myopia develops when the eye is abnormally long - a condition that occurs more often in children and adolescents who spend fewer hours outdoors than non-myopic children.
Speaking of smartphones and computer screens, these and other electronic devices are being attributed to increased cases of non-genetic myopia in adults. Staring at small screens for hours without focusing on distance objects for a few minutes is proving to be unhealthy behavior.
Although there is no scientific evidence suggesting diets or eye exercises can prevent or even slow down the development of myopia, an ample amount of outdoors time is an advisable preventable measure.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Exercise caution with cosmetic eye procedures | By Dr. Frederick Ho
August 14, 2014
In clinical trials, Bimatoprost was found to be an effective treatment of glaucoma and was soon released for medical use. Insignificant at the time, a reported side effect of Bimatoprost was that it lengthened, thickened and darkened eyelashes. As word spread about a prescription glaucoma eye drop affecting eyelashes in a desirable way, some women wanted to use it cosmetically rather than medically. Recently the FDA approved Bimatoprost (brand name Latisse) for conditional cosmetic use. The decision was delayed because it involved approving a medication for its unexpected side effects instead of for its intended clinical treatment of glaucoma.
Not all of Latisse or Bimatoprost’s side effects are welcome.Latisse can produce adverse reactions in some individuals: redness, irritation and darkening of eyelids (in addition to darkened lashes). These conditions disappear when Latisse is discontinued. A rare adverse effect that does not reverse when Latisse is discontinued is the darkening of the iris – the colored area of the eye encircling the pupil. The FDA conditional cosmetic approval includes warnings about contact lens contamination, pregnancy, breast feeding as well as a dispensation prohibition for individuals under eighteen.
Dark, long lashes look even more beautiful when the eyelid is perfectly lined. Permanent eye-lining using tattoo ink can is a relatively safe way to achieve this cosmetic goal. However, as with any tattoo, there are risks associated with infection, allergic reactions to chemicals in the ink, especially if the ink is of inferior quality. Some tattoo ink with high iron content may cause eyelid damage with MRI scan. Excessive temperatures produced by malfunctioning tattoo tools can scar and deform eyelids.
Eyebrows can also be created with tattoo ink. Initially developed for individuals with no eyebrows, the procedure was soon adopted by those wanting to restore partial and faint eyebrows. Today, the procedure is being purchased by people who desire permanent, perfectly shaped eyebrows.
Caution is advised. The same tattoo related risks and caveats associated with permanent eyeliner also apply to eyebrow enhancement: infection, allergic reactions to ink chemicals and scarring.
Color is the number one trait associated with eye beauty. We all have our preferences: blue, green, hazel, brown. Colored contact lenses offer an opportunity to temporarily change eye color. Acquiring decorative color contacts requires an eye exam from a licensed contact lens professional and a valid contact lens prescription. Proper lens cleaning and disinfecting procedures must be followed to avoid sight threatening corneal infection and scarring.
The color of one’s eye can be permanently changed with iris implants. The iris implant was originally developed for patients who lost iris tissue from an injury or never developed it because of a congenital deformity to protect the eye from excessive light and glare. It is a color silicon ring with the preferred color covers only the iris without blocking the pupil. Complications have been associated with iris implants - from light sensitivity to vision loss. Beyond adverse reactions of infections, there’s the dangerous possibility of development of chronic inflammation, damage to the cornea, cataract formation and glaucoma. Iris implants are not approved by the FDA and are strongly discouraged for cosmetic purposes.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
HOMETOWN NEWS
September, 2014
Return to Top of Page
Viera Voice
Dr. Frederick Ho: True family man at heart | By Linda Wiggins
August 2014
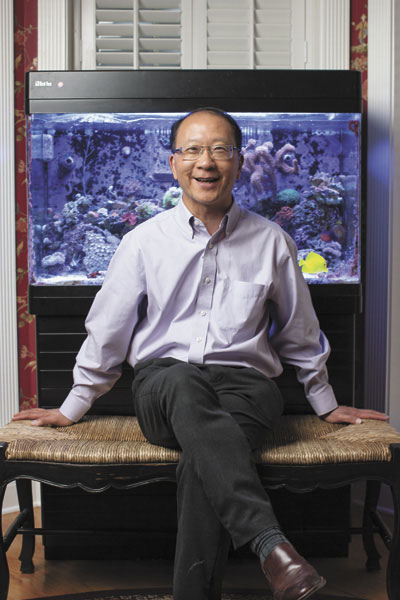 Baby-blue eyes that laugh and dance. Eyelashes so long and curly they touch the eyebrows. Creamy skin with pink-rose colored cheeks marked only with dimples and a smile that curves up at the ends in a perfect bow.
Baby-blue eyes that laugh and dance. Eyelashes so long and curly they touch the eyebrows. Creamy skin with pink-rose colored cheeks marked only with dimples and a smile that curves up at the ends in a perfect bow.
Day in and day out, patients report the things they missed seeing that they didn’t even know they were missing before Dr. Frederick Ho operated on their eyes.
A granddaughter’s tiny face responding to a smile. The sparkles that play out on the surface of the Indian River Lagoon. Road signs that allow for the resumption of driving one’s own car.
“It’s very gratifying. You help restore their vision and they get to enjoy it for life,” said Dr. Ho, MD, FACS, owner of Atlantic Eye MD on Wickham Road in Viera, both a hospital where all manner of eye surgeries take place, and an adjacent ophthalmology clinic where patients are diagnosed and treated.
Dr. Ho has performed multi-focal lens implants for close to a decade, likewise for toric lens implants for astigmatism, both life-altering procedures for the right candidates. Diabetic glaucoma, cross-eye muscle surgery in children, the ever-popular cataract surgery for boomers and seniors — the list is long.
Now as he closes in on three decades of practice on the Space Coast, Dr. Ho may perform surgery to unblock the tear duct of a newborn, great-great-great grandchild of one of his first patients on one day, and the next day, perform cataract surgery on a generation somewhere in between.
 “It’s so nice to see something you did 20 years ago still helping the patient,” Dr. Ho said.
While the letters and the one-on-one thanks he receives from patients are uplifting, there is an even greater gratification he enjoys, that which comes from his wife, Laurie, and their four young daughters.
“It’s so nice to see something you did 20 years ago still helping the patient,” Dr. Ho said.
While the letters and the one-on-one thanks he receives from patients are uplifting, there is an even greater gratification he enjoys, that which comes from his wife, Laurie, and their four young daughters.
“Life is all about them now. That is life’s greatest satisfaction,” said Dr. Ho, who once received gratification aboard the “flying eye hospitals” of the international nonprofit Project Orbis. Before he had a family of his own, he flew to his native China to help entire families of patients with their eye surgery needs, teaching other professionals like him to carry on the skills, thus “teaching a man to fish, rather than giving him a fish.”
His time after work is spent helping his girls, a third-grader and twin fourth-graders at Freedom 7 Elementary School and a seventh-grader entering Holy Trinity Episcopal Academy, with their homework. During the summer and on holidays, he and Laurie take the girls to experience the landmarks, cultures and magnificence of their native United States.
“Like many people we know, we find great joy in opening their eyes to what they can accomplish in life,” Dr. Ho said, “whether that is studies, mastering musical instruments, or discovering, creating new frontiers. They are growing up happy, curious, healthy children.”
Things the couple does not put on the back burner: their own interests, and each other.
For him? Painting with watercolor pastels, tending his saltwater aquarium and its living inhabitants, reading — either on his “handy, pocket-size mini iPad” or, currently in hardback, a copy of “The Proud Tower” by Barbara W. Tuchman, a portrait of the world before World War I. For Laurie: tennis, sculpture, museums.
For both? Once or twice a year they put the kids in summer camp, someplace fun and beneficial, while they travel to see the sights, try new restaurants, stay in love.
“We don’t forget to take time for ourselves.”
For more information, call 321-757-7272.
Return to Top of Page
FLORIDA TODAY
Pot is dismissed for eye care | Dr. Frederick Ho
July 31, 2014
In a 4-3 vote, the Florida Supreme Court approved the wording of a proposed amendment to the state constitution regarding medical marijuana. It will appear on the November ballot. If passed, the state will allow marijuana treatment for "debilitating medical conditions" and for other conditions for which a physician believes its use "would likely outweigh the potential health risks."
Amendment proponents want you to know marijuana reduces intraocular pressure — the leading cause of glaucoma, an inarguably debilitating condition. Marijuana also retards the production of abnormal blood vessels — the leading cause of "wet" age-related macular degeneration, another such condition.
The National Eye Institute, the American Academy of Ophthalmology, the Glaucoma Research Foundation and the National Institute of Health want you to know that the traditional treatments for these diseases significantly outperform marijuana.
In glaucoma, elevated intraocular pressure causes optic nerve damage, reducing peripheral vision and, if left untreated, blindness. In an effort to prevent vision loss, glaucoma is controlled with surgical procedures or prescription eye drops, depending on the type of glaucoma being treated and its severity. A prominent chemical in marijuana — THC (a cannabinoid) — has been shown to reduce the eye pressure temporally in patients with glaucoma.
Inhaled, swallowed or even administered intravenously, the eye pressure reduction is brief, requiring six to eight doses to control pressure over a 24-hour period. Such frequent dosing can alter moods, and impair the mental function and ability to safely operate equipment. Conventional glaucoma eye drop medications are placed in the eye once or twice a day to achieve the same round-the-clock intraocular pressure control with minimal or no side effect.
Marijuana doesn't just lower the eye pressure, it also lowers blood pressure. Reductions in blood flow to the optic nerve can cause damage in glaucoma patients. Whatever relief marijuana provides by reducing intraocular pressure reduction is lost to low blood pressure adversely affecting the optic nerve.
Vision loss can also occur as a result of abnormal blood vessel growth on or near the retina. This condition is often associated with macular degeneration or diabetic eye disease in the retina (diabetic retinopathy). Delicate, fragile vessels grow abnormally due to poorly controlled blood sugar in diabetic patients or inflammation in macular degeneration patients. Blood and serum leak out from a tangled, vascular web. Eventually, this causes irreversible damage to the retina and, if left untreated, rapid vision loss until blindness.
Thankfully, medical researchers have developed drugs that minimize vision loss by inhibiting the growth and promoting the regression of these abnormal blood vessels. Cannabinoids have similar anti-angiogenic properties, but drugs such as Lucentis, Avastin and Eylea significantly out-perform marijuana alternatives.
If an individual has elevated IOP or abnormal vascular growth and is using marijuana to treat nausea, vomiting, loss of appetite, chronic and neuropathic pain, epileptic seizures or multiple sclerosis, medical marijuana's ophthalmic benefits would be a welcome adjunct.
As a primary treatment for any ophthalmic disease or disorder, marijuana has been medically dismissed.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Thyroid disorder triggers trouble for the eyes | Dr. Frederick Ho
May 15, 2014
Thyroid is a butterfly-shaped gland in the neck producing hormones that regulate the rate at which many body systems function as well as their rate of growth. An autoimmune disorder known as Graves' disease mistakenly triggers the immune system to attack the thyroid gland with antibodies. This will often cause the thyroid to become overactive — a condition called hyperthyroidism.
Reacting to different sets of antibodies, thyroid-eye disease is a similar autoimmune disorder that adversely affects the muscles and connective tissues of the eye. The associated swelling and inflammation in these muscles and connective tissues causes eye protrusion, eyelid retraction, double vision and, in rare instances, vision loss.
Not everyone with thyroid disease has problems with their eyes. It is, however, a common enough problem that you may know someone with this condition. Former first lady Barbara Bush and actor Marty Feldman, who played "Igor" in the film "Young Frankenstein," have symptoms associated with thyroid eye disease.
Thyroid eye disease occurs in about one in 20 people with hyperthyroidism. It can also occur in people with an underactive thyroid and, rarely, this condition can even present before the onset of thyroid abnormality. Thyroid eye disease affects patients between the ages of 30 and 50; more women than men, although the most severe cases are seen in men, most older than 50.
Symptoms of thyroid-related eye disease range from mild to severe. The signs and symptoms in an individual can be quite variable, often changing from week to week.
Patients often complain of a dry feeling, irritation and occasional teary eyes. This is usually due to eyelid retraction and protrusion of the eyes.
The "stare" appearance, commonly associated with Graves' disease, is also a result of eyelid retraction. At night, the eyelids sometimes do not completely close, drying the cornea, resulting in discomfort.
Bulging or protruding eyes are due to inflammation and fluid accumulation in the connective tissues, fat and muscles around and behind the eye, pushing the eye outward. In severe swelling of muscles that move the eye, the optic nerve, which connects the eye to the brain, is compressed and vision is diminished. Swelling in the muscles that move the eyes can also lead to double vision.
A common misconception is once the thyroid condition is treated, the eyes will return to normal. The reality is some patient's thyroid-related eye conditions worsen in the months and years after medical treatment. Nevertheless, normalizing thyroid function is an important factor in a patient's well-being.
An ophthalmologist who is knowledgeable in thyroid eye disease can be very helpful in several ways. First, by helping patients get through the time when the eyes are changing, offering solutions to the irritation, tearing and swelling.
Often this may be as elementary as using artificial tears during the day and lubricating ointment at night. Sleeping with one's head elevated by pillows can decrease swelling around the eyes.
Secondly, by determining when thyroid-eye conditions are stable and whether corrective measures are necessary. Most importantly, ophthalmologists protect the eyes from rare, yet possible, sight-threatening problems associated with thyroid disease that necessitates immediate attention.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Sleep apnea can affect your eyes | Dr. Frederick Ho
April 30, 2014
Sleep apnea is a chronic condition that interrupts breathing during sleep. In obstructive sleep apnea, the airway becomes blocked, causing breathing to stop for up to2 minutes. This condition affects more than 12 million Americans. Its symptoms include loud snoring, gasping or choking while asleep, morning headache and daytime sleepiness.
Sleep apnea adversely affects the delicate and fragile vessels in the eye, particularly the retina, by sudden fluctuations of blood pressure and oxygen levels. During undisturbed sleep, the systemic blood pressure decreases slowly. Retinal vessels dilate to match blood flow based upon oxygen and metabolic demands.
In obstructive sleep apnea, oxygen levels drop rapidly and dramatically. Retinal vessels respond by dilating maximally to prevent retinal damage from oxygen deprivation or ischemia. The brain, however, responds to a lack of oxygen in the blood by releasing epinephrine and norepinephrine hormones that cause blood pressure spikes. These repeated hypertensive episodes throughout the night result in nests of micro-infarcts or mini-strokes and damage the retinal tissue.
Sleep apnea accelerates and compounds the abnormalities associated with diabetic damage to the retina. Diabetic patients can develop signs of impaired retinal blood flow and retinal micro-infarcts despite having a healthy blood sugar level. Decrease blood oxygen level in retinal capillaries and eye tissues triggers a release of chemicals that, in turn, could cause macular edema — excessive fluid in the macula — the center of the retina where perception of precise, sharp details of images occurs.
Ischemic optic neuropathy has also been associated with sleep apnea. This condition describes a mini-stroke of the optic nerve, the eye's direct connection to the brain. Optic nerve swelling from raised intracranial pressure is recognized in obstructive sleep apnea patients who often complain of headache upon waking.
More recently, sleep apnea has been identified as an independent risk factor for open-angle glaucoma — elevated pressure inside the eye to a level that damages the optic nerve causing a gradual loss of vision. Sleep apnea patients are nearly two times more likely to have open-angle glaucoma. Individuals who experience sleep apnea are encouraged to be screened for glaucoma.
Floppy eyelid syndrome is one of the most common ocular disorders associated with obstructive sleep apnea. Ninety percent of patients with floppy eyelid syndrome have obstructive sleep apnea. Apnea events prompt a sleeping position shift. The large, elastic upper eyelids become easily distorted and everted when they come into contact with pillow cases. These patients complain of chronic tearing, eye irritation and blurred vision; worse upon waking.
Additionally, apnea interferes with REM sleep — a stage of deep sleep when muscles are maximally relaxed and body systems are at maximum rest. Sleep apnea interrupts this overnight system reset, a condition that adversely affects an individual's physical and mental health.
Obstructive sleep apnea is more common in men than women. Typical apnea patients are middle-aged with a thick neck or narrow pharynx and have a body mass index of more than 28. Sleep apnea suspects also include children with enlarged tonsils, youngsters experiencing daytime sleepiness and adults whose partners report loud snoring.
Following sleep lab evaluations, successful treatments can be implemented to protect patients from the ocular and systemic ravages of obstructive sleep apnea.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
MELBOURNE AWARD PROGRAM
Ho K Frederick MD Receives 2014 Best of Melbourne Award
April 25, 2014
Melbourne Award Program Honors the Achievement
MELBOURNE April 25, 2014 -- Ho K Frederick MD has been selected for the 2014 Best of Melbourne Award in the Ophthalmology category by the Melbourne Award Program.
Each year, the Melbourne Award Program identifies companies that we believe have achieved exceptional marketing success in their local community and business category. These are local companies that enhance the positive image of small business through service to their customers and our community. These exceptional companies help make the Melbourne area a great place to live, work and play.
Various sources of information were gathered and analyzed to choose the winners in each category. The 2014 Melbourne Award Program focuses on quality, not quantity. Winners are determined based on the information gathered both internally by the Melbourne Award Program and data provided by third parties.
About Melbourne Award Program
The Melbourne Award Program is an annual awards program honoring the achievements and accomplishments of local businesses throughout the Melbourne area. Recognition is given to those companies that have shown the ability to use their best practices and implemented programs to generate competitive advantages and long-term value.
The Melbourne Award Program was established to recognize the best of local businesses in our community. Our organization works exclusively with local business owners, trade groups, professional associations and other business advertising and marketing groups. Our mission is to recognize the small business community's contributions to the U.S. economy.
SOURCE: Melbourne Award Program
CONTACT:
Melbourne Award Program
Email: PublicRelations@recognitionawarding.com
URL: http://www.recognitionawarding.com
Return to Top of Page
FLORIDA TODAY
Cataract surgery improves vision, other life qualities | Dr. Frederick Ho
April 2, 2014
A cataract is a clouding of the natural lens in the eye. It is usually the result of aging, which causes proteins in the eye to break down and clump together, affecting the clarity of visual images on the retina.
Initially, cataracts can be tolerated by getting stronger glasses to improve vision. However, when the cataract causes significant visual disability, having it surgically removed is the best option. After the cloudy lens is removed, a clear intraocular lens is implanted, which then becomes a permanent part of the eye. This implant can either be a standard lens or the newer option of multifocal lenses or an astigmatism-correcting toric lens.
Many outcome studies have demonstrated that cataract surgery not only improves vision but also enhances quality of life. Research is showing evidence on safety and possible cognitive benefits for elders.
Cataract surgery also has decreased the risk of falling, hip fractures and car accidents. Perhaps the most striking outcome is that the oldest patients benefited most from cataract removal.
Half of all people older than 80 fall each year, many of whom who suffer hip fractures and are admitted to hospitals and nursing homes. Of those admitted to nursing homes, 40 percent never return home; 25 percent die within 12 months.
Following cataract surgery, research study patients experienced 16 to 23 percent fewer hip fractures than a comparable group who chose not to have cataract surgery (in the same 12 month period).
The greatest reduction of hip fractures occurred in patients 80 and older. The group that most needed to benefit from cataract surgery did so.
We have verification from 400,000 Medicare cataract patients confirming the benefits of cataract surgery extend far beyond improved vision.
Research from Australia and the United States found removing cataracts reduced car crashes. The Australian study examined the relationship of cataract surgery and car crashes of 30,000 surgeries over nine years. There were 13 percent fewer crashes among elderly patients who had cataract surgery with intraocular lens implants compared with cataract patients who chose not to have surgery.
The American study demonstrated elderly patients having cataract surgery were involved in half as many wrecks four to six years later, compared with elderly cataract patients who declined surgery.
A current study is focusing on the relationship between cataract removal and the life-quality improvements in Alzheimer’s patients. Alzheimer’s disease and cataracts are age-related, so it’s not unusual for both conditions to be present in an elderly patient. Ophthalmologists believe the improved vision from cataract surgery is directly related to improving the quality of life for Alzheimer’s patients.
Cataracts might stop one from looking through magazines or sewing. Following cataract removal and a lens implant, these activities can be resumed. The person is stimulated and mentally engaged. Their mood improves.
A study at a Paris hospital examinned 38 female patients in their 80s with mild Alzheimer’s type dementia and debilitating cataracts. Following cataract surgery, half the patients slept better and were less depressed.
A study is looking at whether cataract surgery will improve perception, independent functioning and quality of life in American patients with Alzheimer’s disease.
We will have solid evidence that aside from improving vision, cataract surgery improves social and physical functioning. Elderly patients and their families considering cataract surgery can be advised that the procedure is especially beneficial for older patients; proven to improve the overall quality of their life in addition to restoring their vision.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
ANGIE'S LIST
 Dr. Frederick Ho won the 2013 Angie's List Superior Service Award.
Dr. Frederick Ho won the 2013 Angie's List Superior Service Award.
This is the highest honor given annually to the top 5% of ophthalmologists in Angie's List.
Return to Top of Page
FLORIDA TODAY
Focus On Eyes: Avoid Olympics-sized eye infection with precautions | Dr. Frederick Ho
March 19, 2014
“You hear it called pink eye or conjunctivitis,” explained Bob Costas, host of NBC- TV’s 2014 Winter Olympics coverage. “You have swelling and stinging and burning and, eventually, tearing.”
The irritation associated with this condition initially forced the removal of Costas’ contact lenses. When the infection worsened and spread to his other eye, Costas had to abandon the Olympics anchor desk.
Conjunctiva is the thin, clear membrane that covers and eye’s surface and lines the eyelids, which lubricate the eyes. When irritated, infected or otherwise inflamed, blood vessels in the conjunctiva swell making the eye appear red. Conjunctivitis is caused by a variety of pathogens and allergens: bacteria, virus, fungus, pollen, dust and dander.
Viral infection is the most common form of infectious conjunctivitis, a contagious form of pink eye. This is the same virus that causes the common cold. Symptoms can last from one to two weeks before they disappear. Also contagious, bacterial conjunctivitis can be eradicated (unlike a viral infection) with antibiotic eye drops or ointments in a few days.
The contagious nature of infectious conjunctivitis obliges one to avoid people with pink eyes, to keep hands away from your eyes and to wash hands frequently. If you should need to touch your face around your eyes, always use a tissue. Eye and cheek cosmetics should be replaced.
People who wear contact lenses must clean them very carefully and replace them regularly. If symptoms of conjunctivitis should occur, stop wearing the lenses, as Costas did. If the condition does not clear in a day, consult an ophthalmologist for possibility of a corneal ulcer — a serious sight-threatening infection.
If you live with someone who has pink eye, make sure they are practicing good hygiene, especially washing frequently. Another essential behavior is not leaving things they’ve touched in a place where others might use them. Be aware of items touched by a person with this condition: towels, wash cloths, bedroom linens, telephones, light switches, door handles, computer keyboards and mice, remote controls and any multi-serving beverage and condiment containers.
Noninfectious conjunctivitis is associated with seasonal allergies. The body responds to pollen, mold and dust and dander sensitivity by releasing histamine, which initiates tearing, itching, swelling and redness. Antihistamine eye drops reduce, if not eliminate, these symptoms. Keep your car and home closed. Clean or replace your air conditioner filter often. Avoid hand-eye contact.
If the inflammation is especially severe, an ophthalmologist may prescribe steroid eye drops.
Other conditions cause red eyes. An examination by an ophthalmologist will assure a correct diagnosis and effective treatment.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus On Eyes: Visual complications caused by a stroke | Dr. Frederick Ho
January 8, 2014
The symptoms and degree of visual loss associated with strokes is dependent upon where theblood blockage occurs — in the eye or in the brain.
Ophthalmic strokes particularly affect the retina and optic nerve. The most common symptoms are a sudden, painless, complete or partial loss of vision in one eye and blind spots. Reading suddenly becomes difficult; symbol recognition particularly so.
Without blood-borne oxygen and nutrients, retinal tissue will deteriorate within hours. If the retina’s central artery suffers blockage, a profound and usually permanent loss of central vision occurs because of inhibited blood flow. If a branch retinal artery is occluded, the vision loss is less severe and, more importantly, over time, there is fair chance of visual recovery.
The retinal artery blockage can be caused by a clot or plaque buildup in the blood vessel. When patients have symptoms from central retinal artery occlusion, they may regain some vision within a few hours. Treatments include: inhaling a mixture of oxygen and carbon dioxide that helps dilate the retinal artery and resumes blood flow, removal of a small amount of fluid from the front of the eye that allows the clot to move to a branch of retina artery, and intravenous administration of a clot-dissolving drug.
The optic nerve is also nourished by blood. If any blockage has developed in the artery or its branches along its pathway, visual loss may occur. This condition is termed ischemic-optic neuropathy. It may be sudden or it may develop over a few days.
In addition to blockage, the optic nerve and retina may also be adversely affected by an inflamed, swollen artery. The swelling in the artery walls from inflammation restricts blood flow. When this condition occurs, it is referred to as giant cell or temporal arteritis. Its symptoms include headache, scalp tenderness (particularly around the temples) and jaw pain. Vision loss generally occurs in one eye but can also develop in the other eye if the inflammation goes untreated.
Currently, little can be done to repair optic nerves damaged by strokes. Controlling blood pressure, cholesterol and blood sugar are prominent preventative measures. Exercise and not smoking also reduce the risk of stroke. Arteries in the neck and the heart can be examined as possible sources of blood clots.
A blood test and biopsy of the temporal artery are recommended if temporal arteritis is suspected. Temporal arteritis is treated with high doses of oral steroids to relieve inflammation and prevent vision loss in the other eye.
Strokes in the brain can cause peripheral vision problems and double vision. The degree of peripheral field loss depends on the part of the brain where a stroke occurs. Double vision is the result of eye muscle weakness following damage to the brain or nerves controlling the eye muscle.
Prompt evaluation and treatment at a hospital with a certified stroke treatment center offers the best opportunity for recovery. Anyone experiencing visual changes associated with a stroke should be examined by an ophthalmologist who evaluates and helps alleviate as many visual complications of a stroke as possible.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Diabetes can endanger vision | Dr. Frederick Ho
November 25, 2013
The growing prevalence of diabetes reflects the surging rates of obesity. Diabetes is one of the leading causes of blindness in the United States and is preventable with regular eye examinations and timely treatments.
All people with diabetes — whether insulin dependent or not — are at risk of diabetic eye disease, specifically diabetic retinopathy (disease of the retina). Between 30 to 40 percent of diabetic patients have some form of retina disease. To protect vision, patients with diabetes should have a comprehensive dilated-eye examination at least once a year.
Diabetic retinopathy occurs when the disease damages the tiny blood vessels inside the retina. The retina in the back of the eye functions like the film in a camera. A healthy retina is necessary for good vision. The damaged blood vessels leak fluid into the center of the retina — called macula — where sharp, straight-ahead vision occurs. The fluid makes macula swell, blurring vision. This condition is called macular edema.
When diabetic retinopathy progresses, blood vessels are blocked, depriving areas of retina with their blood supply and nourishment. This triggers the growth of fragile abnormal blood vessels. This is called proliferative diabetic retinopathy. The abnormal vessels have thin walls and they leak blood, causing hemorrhaging inside the eye, which causes severe visual loss.
When macular edema is detected, laser surgery is recommended. The ophthalmologist apples focal laser treatment in the areas of retinal leakage surrounding the macula. The treatment stabilizes vision and prevents risk of vision loss by 50 percent. The procedure is usually performed in the office.
The condition requires extensive laser surgery. Many laser burns are applied in the areas of the retina away from the macula, causing the abnormal blood vessels to shrink. The treatment helps to save the central vision, although patients may experience a decrease of side and night vision, plus the inability to distinguish colors.
If the hemorrhage from proliferative diabetic retinopathy is severe, a surgical procedure, called vitrectomy, is needed to evacuate the blood from the inside the eye.
Recently, medication has been used to treat diabetic retinopathy. The medications — such as Lucentis, Avastin or Eylea — work by blocking a protein that stimulates the abnormal blood vessel growth in the eye. The agent reduces fluid leakage and interferes with growth of unwanted blood vessels in the retina. It is useful in the treatment of diabetic macular edema and proliferative diabetic retinopathy. The injection is typically performed with numbing drops in the ophthalmologist’s office at regular intervals. It may be combined with laser to achieve the best results.
Everyone with diabetes is urged to have a comprehensive eye examination at least once a year. Medicare and most health insurance plans recognize these examinations as medical necessary. Studies have shown that better control of blood sugar levels slows the onset and progression of diabetic retinopathy. Controlling blood pressure and cholesterol can reduce the risk of vision loss.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Shingles virus can also endanger vision | Dr. Frederick Ho
October 8, 2013
Shingles is a painful skin and nerve condition caused by the same virus responsible for chickenpox. The virus is called varicella when in children, herpes zoster when it recurs in adults. If this virus infects the skin around an eye or the eye itself, it’s termed herpes zoster ophthalmicus (frequently referred to as HZO). People who develop HZO usually had chickenpox during childhood.
Following the initial infection, virus particles remain in the body’s nerve cells where they lay dormant for years. Some time later, the virus is reactivated causing a skin rash commonly called shingles. Shingles can appear on any part of the body. The torso is the most common site. The forehead is second, threatening sight when it travels into or even near the eyes.
More than 90 percent of adults have either had chickenpox or been exposed to the herpes zoster virus. Medical researchers believe as the body ages, the potency of its immune system declines. At a certain age, the immune system is unable to suppress virus reactivation. Medical experts are unable to predict when the virus will reactivate or, among patients with a reactivated virus, where herpes zoster will appear.
If you have a rash with small blisters on your forehead or around your eyes, you may have HZO. When zoster blisters appear at the tip of the nose, the likelihood of HZO is significantly higher. In addition to pain, flu-like symptoms usually precede a zoster rash by a few days: fatigue, malaise, low-grade fever coupled with numbness and tingling in the area of future blister eruption. Forehead rashes become blistered, sometimes so severely they the skin dies (necrosis).
Corneal damage is the most common complication of HZO. Impairments range from mild irritation and blurry vision to permanent corneal swelling and scarring. Iritis (inflammation inside the eye) can cause pain and photophobia, quicken cataract development, spike in eye pressure (glaucoma) and, in rare cases, harm the retina. Eye muscle paralysis can develop as the result of inflammation in the nerves and muscles with the person seeing double.
Antiviral medications, such as Famvir, Valtrex or Acyclovir, represent the initial treatment. Steroid eye drops or tablets may be prescribed to reduce inflammation. Glaucoma eye drops may be necessary when there is elevated intraocular pressure. If the patient is experiencing pain, analgesic medications may be prescribed.
Patients recover from uncomplicated HZO in a few weeks. If complications occur, recovery takes more time. The age of a patient affects recovery time as does the patient’s health. Patients with HIV, diabetes or cancer experience extend and complicate recoveries.
Chronic pain from nerve damage caused by herpes zoster (post herpetic neuralgia) affects about 20 percent of shingles patients, the elderly often more severely.
Patients with herpes zoster ophthalmicus can transmit the varicella-zoster virus. People who have not had chickenpox must avoid patients with HZO –especially unvaccinated children and pregnant women.
Shingles endanger the eyes when the herpes zoster virus causes inflammation in the delicate ocular tissues, muscles, nerves and blood vessels. Fortunately, an effective shingles vaccine is now available for adults. It decreases the chance of developing shingles and post herpetic neuralgia by half.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
HOMETOWN NEWS
October, 2013
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: Dry eyes a common malady on the coast | Dr. Frederick Ho
August 14, 2013
Coastal Florida, with its sunlight, sand, fine soil and sea breeze, is exceptionally harsh on our eyes.
We’re likely to face particulate air every time we venture outside. Staying indoors may not bring relief,
especially from large, minimally filtered air-conditioning and heating systems. If you’re focused on a
computer or TV screen, you’re blinking less, reducing the delivery of protective moisture to the ocular
surface.
Antihistamines, decongestants and diuretics purposefully reduce body fluids. Unfortunately, that also
includes the protective tear film. Anti-depressants, tranquilizers, birth control and blood pressure
medications all have dry eyes listed as a possible side effect.
Every year, 25 million Americans complain to ophthalmologists of red, itchy, stinging, burning eyes that
are sensitive to light or have a scratchy, gritty or foreign body sensation. It’s allergies, they say, but it is
probably dry eye disease. Mild cases of dry eyes are annoying. Moderate and severe cases can be
painful.
In a perfectly working eye, the lacrimal (tear) and meibomian (oil) glands in eyelids secrete a mixture of
mucus, oil and water every time we blink. The tear film serves as a protective barrier between the cornea
and exterior environments. Dry eyes occur most often when these secretions are of insufficient quantity or
of deficient quality. The quantity and quality of tear production declines as we age. They also decline as a
result of anatomical or systemic disorders.
The best possible tear film will not be dispensed if an incomplete blink fails to launch secretions from the
meibomian and lacrimal glands. It may not be adequately distributed atop the ocular surface because of
abnormal blinking — usually attributed to eyelid or cornea abnormalities or inflammation of the
conjunctiva.
Dry eyes have been associated with Sjogren’s syndrome among rheumatoid patients as well as hormonal
and thyroid disorders. They have also been identified as a side effect of refractive eye surgery.
Environmental-induced dry eyes can be prevented by protecting your eyes from particulate air with
glasses and adding over-the-counter artificial tears at the first indication of dry eye symptoms.
Some contact lens wearers may have to reduce their hours of lens wear or stop altogether due to
discomfort caused by dry dyes. Warm compresses will usually normalize oil flow from blocked glands.
Those who awaken with a gritty sensation in their eyes benefit from a bedtime application of a lubricant
instead of drops. Over-the-counter tear drops should not be used more than six times daily, because they
contain detergent-based preservatives that can accumulate and harm the eye. Individually packaged
artificial tears are available for people sensitive to preservatives or severe dryness requiring frequent
dosing.
Dietary omega-3 fatty acids help improve the quality of oils in the film tear. Regular diet of fatty fish and
oral supplements of fish and flax seed oils are encouraged for patients with dry eyes.
If these remedies are not solving the dry eye symptoms, an examination by an ophthalmologist is highly
recommended to confirm the diagnosis and identify any other treatable conditions, such as eyelid
abnormality or chronic low-grade infection of eyelids. Short-term steroid drops may be prescribed for
symptomatic relief. Restasis is an emulsion that increases natural tear production and is a successful
long-term therapy for many patients.
Severe cases of dry eyes may require eyelid reconstruction, thermo-cautery or a temporary plug in the
tear drainage duct. This procedure not only conserves naturally produced tears, it also extends the time
artificial tears can moisturize the eye.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Focus on Eyes: Ocular migraines fairly uncommon | Dr. Frederick Ho
August 1, 2013
Migraines are a common neurological condition affecting 15 percent to 20 percent of the population and experienced more often by women than men.
Migraines that cause only a headache felt in one or both sides of the head lasting for hours are classified as a common migraine or a migraine without aura. A migraine that begins with visual symptoms like zigzag lines, flashing lights expanding to one side of your vision and followed by a pounding, one-sided headache (usually) is called a classic migraine, or a migraine with aura.
Ocular migraines are painless, temporary visual disturbances involving one or both eyes. It is a relatively uncommon condition affecting about one of every 200 people who have migraines. Some doctors call them retinal, or ophthalmic, migraines. Although the initial attack can be quite frightening, ocular migraines are typically harmless and self-limiting, disappearing within half an hour without medication.
People experiencing an ocular migraine may see a variety of symptoms. A small blind spot could appear in your central vision surrounded by bright flashing lights or jagged lines, or “heat waves.” The blind spot gradually enlarges, covering the upper or lower portions of your field of vision, or it could cover it entirely. This episode of visual disturbance is temporary; occasionally ending in a few minutes but usually lasting up to 30 minutes. Permanent visual loss is a rare complication of migraines.
Ocular migraines are believed to have the same causes as migraine headaches. Inflammatory substances are released deep in the brain and around the blood vessels of the head and brain. Imaging studies reveal changes in blood flow to the brain during ocular migraines and visual auras. How this happens is not yet known, neither is what brings about the resolution of the visual disturbance.
Ocular migraine patients usually have a family history of migraine headaches or have suffered previous migraine attacks with or without auras. They are more prone to be car sick or have cold hands and feet.
To diagnose an ocular migraine, an ophthalmologist must exclude other conditions that have similar symptoms such as:
• Vitreous separation or vitreous detachment. Vitreous is the gel-like substance inside the eye that can pull away from the retina causing flashes or floaters.
• Retinal tear or retinal detachment. Visual symptoms persist and require medical attention.
• Amaurosis fugax. Transient blindness due to decreased blood flow to the eye. Medical evaluation determines the underlying cause.
• Giant cell arteritis. Arterial inflammation that can lead to stroke and blindness. Prompt diagnosis and treatment is needed.
• Medication side effects.
Because ocular migraines are generally harmless and resolve on their own within a half-hour, no treatment is usually required. Should one occur while driving, pull off to the side of the road as soon as safely possible. Discontinue any activities involving cutting or sharp objects.
Whenever unusual visual symptoms are experienced, a comprehensive examination by an ophthalmologist is highly recommended.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Protect your eyes during sports, recreation | Dr. Frederick Ho
July 3, 2013
Eye injuries from sports and recreational activities are relatively common, but not inevitable. In fact, 90 percent of serious eye injuries are preventable when using proper, protective eyewear.
Eye injuries can occur from objects hitting the eyes and from head trauma that does not necessarily involve direct contact with an eye —heads hitting stationary objects, participants colliding, a boxing blow to the head or heading a soccer ball.
Serious eye injuries from these collisions include torn or detached retinas, optic nerve damage and orbital fractures. Sports most associated with these injuries are boxing, martial arts, hockey, lacrosse and baseball.
Basketball and racquet games cause numerous, but less severe, eye injuries among boys. Gymnastics, soccer and field hockey cause a majority of eye injuries among girls.
Of all recreational endeavors, the activity associated with the highest number of eye injuries is fishing.
There are two realms of sports-related eye injury prevention: mental and physical.
Carefully observing your sporting or recreational environment is smart. What objects are flying around you? Balls, pucks, fishing tackle? What stationary objects are at eye level? Is there a tree, wall or pole your head could hit? Is there anything moving on the ground tall enough to hit your head; an opposing player, perhaps?
Protective eyewear for all contact sports is highly recommended. Sunglasses and eyeglasses are not considered protective eyewear. In baseball, ice hockey and lacrosse, a helmet with a wire facemask or a lightweight, shatterproof, polycarbonate face shield should be worn at all times. Protective polycarbonate lenses in glasses and goggles or face shields should be worn when playing basketball, soccer, field hockey and racquet ball.
Choose eye protection equipment approved by a sport’s governing body or which has met or exceeded the American Society of Testing and Materials standards. Hockey face masks should be approved by the Hockey Equipment Certification Council or the Canadian Standards Association.
Protective glasses or goggles with UV protection should be worn when snow or water skiing. They help shield the eyes from sunburn and glare.
Signs of eye injuries include pain, blurry vision, protrusion from the eye socket, unusual pupil size or shape, bleeding or blood in the eyes, decreased eye movement, and nicks, cuts or bruises in the eyelids.
There is no such thing as a minor eye injury. A significant relationship exists between expedient treatment and healing. Vision loss is more often associated with delayed medical attention than it is to the severity of the injury. Accidents resulting in vision loss only a generation ago are recoverable today provided the injured eye is promptly seen by an ophthalmologist. If unavailable, an urgent care center or hospital emergency department is the next best course.
Individuals with decreased vision or loss of use in one eye should avoid contact, impact and racquet sports. Instead, choose sports like swimming, cycling and running. Recreational activities such as bowling and dancing minimizing the chance of eye injury.
With foresight, warmed-up muscles and eye protection, we can stay healthy while enjoying sports and recreation.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Proper handling of contact lenses reduces infection risk | Dr. Frederick Ho
June 19, 2013
Although millions of people safely use contact lenses every day, eye infections are a potential risk.
The most serious infection related to contact lens use is a corneal ulcer(keratitis), an infection of the
transparent tissue in front of the iris and pupil. Bacteria, fungi and amoeba can all cause contact
lens-related keratitis. Corneal ulcers can scar the cornea and impair vision.
In severe cases, corneal ulcers can result in scarring and damage that leads to intraocular complications,
including the need for a corneal transplant.
Symptoms of contact lens-related infections may include redness, pain, tearing, increased light sensitivity,
blurry vision, discharge, swelling or a foreign body sensation. Contact lenses should be removed and an
ophthalmologist quickly consulted should any of these symptoms occur.
Risk of infection varies depending upon the type of contact lens. Rigid or gas-permeable lenses fit
comfortably over the cornea yet allow sufficient oxygenation of corneal tissue. They are less likely to be
associated with an eye infection than any soft contact lens.
Extended wear lenses are associated with more infections than daily-wear soft contacts. These lenses are
continuously worn for one or two weeks. Similarly, sleeping overnight with contact lenses increases the
risk of keratitis. Contact lens contamination and related eye infections are significantly minimized by
wearing single-use, soft lenses that are disposed of daily.
Regardless of the type of contact lens chosen, the best way to avoid eye infections is to follow proper lens
care guidelines as prescribed by your eye care professional; particularly, a rub and rinse step in the
lens-cleaning process, considered by experts to be a superior method of cleaning, even if the solution
being used is a “no-rub” variety. Lenses are rubbed then rinsed with solution before soaking.
Safe handling and cleaning of contact lenses help minimize the risk of keratitis. Contact lens wearers must
clean and disinfect their hands prior to handling.
Contact lenses should not be rinsed with or stored in water (tap or sterile) or wetted with saliva (unsterile).
Saline solutions are not disinfectants. Contact with water must be minimized, including removal prior to
swimming or bathing in hot tubs.
Infection prevention also begins with regular eye examinations, typically on an annual basis, when an
ophthalmologist can ensure the lens prescription is correct and the fitting precise as he or she evaluates
the overall health of each eye.
Should keratitis be diagnosed, an ophthalmologist usually scrapes a small sample of the corneal ulcer to
culture the infectious agent. Bacterial keratitis is treated with frequent applications of antibiotic eye drops.
Antifungal drops and pills are necessary for fungal ulcers. Some fungal keratitis and amoebic keratitis
caused by Acanthamoeba are not always responsive to medication. Surgical removal of the infected
cornea may be necessary to restore vision.
Keratitis is a serious infection that can rapidly progress. Contact lens wearers need to recognize the
symptoms of infection and realize seeking prompt medical attention can prevent vision loss.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
The eyes are a window to your health | Dr. Frederick Ho
April 24, 2013
Unlike our internal organs, the eye is visible and accessible to detailed
microscopic examination. Because the body’s systems are interconnected,
changes in the circulatory, endocrine, immune and nervous systems are
frequently manifested in the eyes. Blood vessels, tissues and nerves in the
eye are very small and delicate. Their conditions can paint a remarkably
accurate picture of what is occurring in the body. Many health conditions
are visible to an experienced ophthalmologist long before a person
experiences symptoms.
Elevated blood pressure causes hardening and narrowing of blood vessels
affecting circulatory efficiency. This leads to focal ischemic whitening of
the retina known as cotton wool spot. Severe or malignant hypertension
often results in damage to the optic nerve from ischemia and visual loss. An
experienced ophthalmologist can see these abnormalities and refer patients
for treatment of hypertension, possibly preventing other complications such
as kidney failure, heart attack and stroke.
Atherosclerosis is a major risk factor for cardiovascular disease and stroke. A gradual accumulation of plaque
(cholesterol) inside anartery decreases bloodflow to vital organs. A small piece of plaque or embolus can break off
and migrate into the eye. An ophthalmologist can see these miniscule clots inside the retinal vessels before a major
stroke occurs.
Elevated blood sugar levels in a diabetic patient can damage delicate blood vessels within the eye. Swollen, inflamed
vessels leak or rupture resulting in retinal hemorrhages and edema. Macular edema and blurry vision result when
these fluids enter the macula — the center of the retina where perception of precise, sharp details of images occurs.
All these events are signs of diabetic retinopathy that can damage the eyes before a patient notices a change in
vision. A dilated eye examination may reveal early signs of diabetic eye disease, helping an ophthalmologist prevent
vision loss.
Circulatory diseases and diabetes are not the only hidden conditions discovered by ophthalmologists. Medical
researchers have identified the occurrence of small, harmless freckles in the retina as a clinical marker for familial
adenomatous polyposis — a congenital condition of early onset, accelerated polyp growth in the colon; many
becoming malignant by age 30. Medical researchers believe these retinal lesions are caused by the same genetic
mutation that produces the colon polyps. The ophthalmic term for this retinal occurrence is congenital hypertrophy
of the retinal pigment epithelium. Early diagnosis of FAP allows immediate treatment of malignant colonic polyps.
The eye is connected to the brain via optic nerves. Strokes, brain tumors and aneurysms can affect peripheral visual
fields, cause double vision and decrease visual acuity. Sudden visual loss from optic neuritis or inflammation of the
optic nerve can be the first symptom of multiple sclerosis. The ophthalmologist, neurologist and neurosurgeon
working together as a team help alleviate damage to the nervous system.
Initial symptoms of autoimmune diseases like lupus and arthritis may be ocular pain, swelling and blurry vision.
Cytomegalovirus in the eye occurs in immunocompromised or HIV positive patients. An ophthalmologist observing
these ocular findings can guide patients to specialists in rheumatology or infectious diseases.
The eyes are the window not only to the soul, but also the health of the body. Ophthalmologists are playing an
increasingly important role in the diagnosis of nonocular diseases and disorders.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Some medications can induce vision problems | Dr. Frederick Ho
April 3, 2013
Read any patient information sheet regarding prescription medications, and you’re likely to see “blurred vision”
listed as a possible side effect. Tissues and vessels inside the eye are very delicate and can be sensitive to chemicals
in drugs that are prescribed for nonocular conditions.
Not every patient who’s prescribed a medication with a possible ocular side effect will experience it. The warning
states possible, not probable. To learn the types of visual problems reported in patient trials and the percentage of
patients who experienced each type of problem, ask your pharmacist for the printed clinical pharmacology inside or
attached to the medicine’s container. Locate the bold letter heading of “Adverse Reactions.”
Here are several commonly prescribed medications that have well-known ocular side effects:
• Cortisones or steroids, commonly prescribed for inflammatory disorders and adrenal deficiency, can cause cataracts
and glaucoma. Cataracts are medically categorized as an age-related disorder. The older you are, the more likely you
are to develop cataracts. Medicinal steroids or athletic performance-enhancing steroid use can cause cataracts in
people significantly younger than the average onset age. Steroids can cause an elevation of intraocular pressure that,
in turn, damages the optic nerve — the defining feature of glaucoma.
• Amiodarone (Cordarone or Pacerone) is a very effective heart rhythm medication and is associated with deposits
on the cornea. This does not interfere with vision, and the deposits disappear when Amiodarone is discontinued. Less
convincing is the connection with ischemia (decrease blood flow) in the optic nerve with Amiodarone. Elderly
cardiac patients using these medications have reported color anomalies, decreased visual acuity, “shining” and glare
problems.
• Urology patients being treated for erectile dysfunction with drugs like Viagra (sildenafil), Cialis (tadalafil) or
Levitra (vardenafil) need to keep an eye out for changes in color perception, increased light sensitivity and blurred
vision. Vision loss has been reported, but a causal relationship between these drugs and an ischemic event in the eye
has yet to be proven.
• Drugs used in the treatment of benign prostate hypertrophy, such as Tamusolin (Flomax), Alfuzosin (Uroxatral),
Doxazosin (Cardura) and Terazosin (Hytrin) have been linked to floppy iris syndrome. During cataract surgery, the
floppy iris tends to prolapse out of the wound and pupillary constriction occurs, increasing the risk of cataract
complications. Knowing the patient’s medication history, eye surgeons can be prepared for floppy iris syndrome,
significantly reducing the risk of complications with appropriate surgical techniques.
• Cancer researchers report that cataracts, impaired visual acuity and eye irritation are the top ocular side effects
associated with chemotherapy treatment of breast cancer. A leading breast cancer medication has an adverse,
vision-related side effect named after it — Tamoxifen retinopathy. This condition involves small cysts, swollen
macula tissue and hemorrhaging contributing to vision loss.
• Because chemotherapies are toxic to rapidly dividing cells, they also can be harmful to cells in the conjunctiva and
cornea. Dry eyes resulting from conjunctival and corneal cell damage usually can be treated with lubricating drops.
• Hydroxychloroquine (Plaquenil) is used for the treatment of rheumatoid arthritis, lupus and various inflammatory
diseases. Hydroxychloroquine crystals have been found in tears, which may aggravate dry eyes. In the retina, that
may cause visual abnormalities. Patients should have a complete, dilated ophthalmic examination within one year of
starting this medication. An annual eye examination, including central visual field and optical coherence
tomography, helps detect any visual and retinal changes.
Vision problems you believe are related to a medication should be brought to the attention of the prescribing
physician. There may be an equivalent drug that does not induce this side effect. If there isn’t, ask your
ophthalmologist’s opinion. What’s tolerated as a minor side effect could be far more serious.
Dr. Frederick Ho is a board-certified ophthalmologist and medical director of Atlantic Eye MD and Atlantic Surgery
and Laser Center, 8040 N. Wickham Road, Melbourne. For an appointment, call 321-757-7272 or learn more by
visiting AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Sun exposure can threaten vision | Dr. Frederick Ho
March 27, 2013
You know ultraviolet light deteriorates our skin and excessive exposure will burn it. Did you realize the same
consequences occur in your eyes, including the retina? In light of our abundance of sunshine, it is essential we shield
our eyes from ultraviolet light with sunglasses, broad-brimmed hats or visors and use sunscreen on the skin
surrounding our eyes including the lids.
Boaters, anglers, golfers, swimmers and skiers need to be aware that ultraviolet glare reflected off water and snow
doubles your exposure to ultraviolet light; sun down, water up.
Although sunlight exposure does not cause cataracts, it can affect the severity and lower the age of onset. The same
is true for age-related macular degeneration. It is also a contributing factor of dry eye. Medical researchers believe
ultraviolet light is directly related to the presence of abnormal tissue on the conjunctiva — the clear membrane
covering the white of the eye. Two of the most common growths are pterygium and pinguecula.
A pterygium (tur-i-gee-um) is a pinkish, triangular, elevated growth on the conjunctiva extending onto the cornea —
the clear, protective outer covering of the pupil and iris. Most pterygia are small and require no treatment unless they
become inflamed. These pterygia may be irritating and annoying. An unusually large pterygium can affect vision by
occluding part of the pupil or altering the shape of the cornea causing an astigmatism — light rays unable to
precisely converge on the retina.
Pterygium development increases as exposure to ultraviolet light increases. People aged 20 to 40 have the most cases
of pterygium onset than any other group and men are twice as likely to present pterygia as women.
If a pterygium adversely affects a patient’s vision or is repeatedly inflamed, it can be surgically removed.
Ophthalmologists believe a pterygium begins as a pinguecula. A pinguecula (pin-gwek-u-la) is an elevated,
yellowish growth in the conjunctiva that does not encroach upon the cornea. Pinguecula are usually small and
confined to a part of the eye not responsible for vision.
Avoidance of ultraviolet light as well as dust, dirt, sand, heat, wind and airborne pollution such as exhaust and
chemical fumes is recommended to maintain optimum eye health beyond the potential development of pterygia and
pinguecula.
Excessive sunlight exposure is also a major risk factor for basal cell, squamous cell and malignant melanoma of the
eyelids. If there is a raised bump, skin color change or unexplained loss of eyelash, it is important to consult an
ophthalmologist promptly. The best outcome for treatment of eyelid tumors is achieved through early diagnosis and
complete excision of all the tumors.
Dr. Frederick Ho is a board-certified ophthalmologist, a fellow of the American College of Surgeons and the
American Academy of Ophthalmology. He is the medical director of Atlantic Eye MD and the Atlantic Surgery and
Laser Center in Melbourne. His office is at 8040 N. Wickham Road in Melbourne. To make an appointment, call
321-757-7272. Visit his website at AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY
Diet plays key role in eye health | Dr. Frederick Ho
February 20, 2013
A diet most beneficial for optimum eyesight emphasizes fish, nuts and dark green leafy vegetables. Also vegetables
rich in lutein, zeaxanthin and carotenoids like carrots, kale, spinach, broccoli, corn, peas, tomatoes, dark lettuce,
turnip, collard and mustard greens, squash and pumpkin. Oranges and tangerines are good as well.
Medical researchers have devoted many years looking at the relationship between nutrition and age-related eye
diseases, most notably macular degeneration and cataracts. The effect of diet on the development and severity of
age-related macular degeneration (AMD) is the more significant.
The macula is the central area of the retina where perception of fine detail occurs. AMD causes almost half of all
cases of vision loss in people older than 40. Its prevalence increases again for people older than 60 and significantly
climbs again for people older than 80. Nearly 1.75 million Americans have AMD.
Degeneration occurs when macula cells are damaged by constant exposure to high-frequency light waves (blue and
ultra-violet) and oxidation residue from the prolific cellular activity in the eye. There are two chemicals highly
concentrated in the macula that help protect the macula from premature deterioration — lutein and zeaxanthin.
Foods rich in lutein and zeaxanthin are led by kale and spinach. Broccoli, corn and peas contain these nutrients but in
lesser amounts per serving.
The first Age-Related Eye Disease Study (AREDS1) in 2001 evaluated a supplement with vitamins C and E,
beta-carotene, zinc and copper. The results touted a significant link to risk reduction of moderate to advanced
macular degeneration but did not affect the probability of developing AMD.
A second study (AREDS2), concluding in December 2012, uses a supplement with lutein, zeaxanthin and omega-3
oils (DHA and EPA). Preliminary results show this combination does lower onset risk as well as significantly
reduces the probability of a patient’s moderate macular degeneration progressing to an advanced stage of severity.
Effective nutritional supplements are important for age-related diseases because our nutrient absorption efficacy
through food decreases as we age. The high concentrations of lutein and zeaxanthin in the macula also decline with
age, so supplements with lutein, zeaxanthin and omega-3 oils are especially valuable for AMD patients and people
with a family history of the disease.
Blood vessels and tissue fibers in the retina are very small and fragile, extremely sensitive to abnormalities such as
swelling and leakage (conditions caused by inflammation). The prolific activity inside the eye requires optimal blood
flow for adequate oxygenation, nourishment and repair as well as efficient lymphatic removal of metabolic waste.
Minor obstructions and impediments can cause major problems. Elevated blood sugar from excessive carbohydrates
and cholesterol from processed foods containing mono and polyunsaturated fats will impede and obstruct and
eventually deteriorate and degenerate the macula.
Avoid these foods and eat plenty of fish, nuts and dark leafy greens.
Dr. Frederick Ho is a board-certified ophthalmologist, a fellow of the American College of Surgeons and the
American Academy of Ophthalmology. He is nedical director of Atlantic Eye MD and the Atlantic Surgery and
Laser Center in Melbourne. Dr. Ho’s office is at 8040 N. Wickham Road. To make an appointment, call
321-757-7272. To learn more about the personalized eye care, visit AtlanticEyeMD.com.
Return to Top of Page
FLORIDA TODAY, HEALTH and MEDICINE MAGAZINE
Excellence In Ophthalmology | Dr. Frederick Ho
January 21, 2013
Click to view PDF version
Return to Top of Page
FLORIDA TODAY, HEALTH and MEDICINE MAGAZINE
Dr. Frederick Ho Celebrates 25 Years of Serving Brevard County
November 19, 2012

Click to view PDF version
Return to Top of Page
VIERA VOICE
Dr. Frederick Ho with his wife, Laurie, celebrate 25 years of success in local business.
October, 2012

The staff at Atlantic Eye MD and Atlantic Surgery Laser Center include Krista LeFeur, Claudia Moore, Tiffany Vachon, Pamela Wisniski, Diane Ortez, Ellen Buffington and Denise Ketchum.
Dr. Ho's anniversary party on August 24 featured finger foods, live harp music and a free T-shirt for every guest.
Return to Top of Page
FLORIDA TODAY, HEALTH and MEDICINE MAGAZINE
Dr. Frederick Ho Celebrates 25 Years of Progress in Ophthalmology
September 17, 2012
Click to view PDF version
Return to Top of Page
FLORIDA TODAY NEWSPAPER
Ophthalmologist Among Leaders in His Profession
Feb 23, 2012
Ophthalmologist and eye surgeon Dr. Frederick Ho has reached the top of his field for successful treatments including cataract surgery, multifocal lens implants, laser surgery, diabetic eye diseases, glaucoma and macular degeneration.
He has been named a U.S. Top Doctor and Top Ophthalmologist according to the Consumer's Guide to Top Doctors and Consumer's Research Council of America, respectively, but it is his passing on that knowledge with colleagues in the East that sticks in his mind the most.
In the 1990s, Ho, from Hong Kong, instructed doctors from China in a jet specially equipped with an operating room as part of Project ORBIS.
"They wanted to spread the latest knowledge about ophthalmology, to train their surgeons so they could help their own patients," he said. "It was very exciting to be able to share this important information."
Ho talks about his longtime career in Brevard County and how innovations and the aging of baby boomers is expected to increase demand in his specialty.
QUESTION: Where and when did you choose your specialty?
Ho: During medical school. Eye surgery is very intricate and very challenging, but the most important thing is I thought I would like helping people see better. It's very gratifying.
Q: What are some of the major innovations that have occurred during your career?
Ho: The advancement in the treatment of cataracts. What used to be a procedure where you would stay overnight in the hospital is now something where it can be done outpatient and you can go home the same day with much less recovery time. Other innovations including the multifocal lens implant for distance and near vision and procedures that can correct astigmatism.
Q: Of those innovations, which one has made the biggest impact on patient outcomes?
Ho: I would say the multifocal lens implant or the lens implant in general. They've been around a long time, but the technology, and therefore the quality, continues to improve and the success rate of the surgery continues to improve. Technology continues to improve. We make smaller incisions for faster healing.
Q: What is on the horizon in your field?
Ho: The use of lasers for cataract surgery, but the big thing is stem cell treatment for macular degeneration. It has been performed successfully on one patient and now it has to be tried on a group in clinical trails for approval by the FDA. There's no way of knowing but I think it could be approved for general use in like five years. We're very successful in treating cataract but now we're making progress in the treatment of macular degeneration.
Q: How long have you practiced in Brevard County and is it a good place for your specialty?
Ho: I've been here 25 years. I'm very happy here because most of my patients are very pleasant and have good outcomes.
Q: Who is your typical patient these days?
Ho: Most are over age 50, but I do occasionally treat a younger person. It's a full range and that's what makes ophthalmology interesting because I do everything.
Q: Have increases in longevity made eye surgery more likely for patients older than 80?
Ho: We have made tremendous progress in making surgeries less traumatic with good outcomes, so really there is no hesitation, even up into their 90s, because they want to see well. The surgery is not stressful. I've even performed surgery on an 100-year-old with a good outcome.
Q: What charitable organizations do you work with now?
Ho: I work with the Brevard Health Alliance, The Lupus Foundation and the Association for the Advancement of the Blind and vocational rehabilitation.
Q: What is the most difficult part of your job?
Ho: The most difficult case is telling parents that you can not improve their child's vision. That's hard, especially for a child, because they have a long life ahead of them. With conditions like lazy eye, you have a window of time to treat and after that, not much can be done. They usually come out in screenings but kids can memorize the eye chart. And with people born with a deformity like defective optic nerve, there's nothing I can do.
Q: Favorite part?
Ho: Helping people see better. You can't get any better than that because it improves their quality of life so much.
Dr. Frederick Ho, ophthalmologist
Hometown: Hong Kong
Family: Wife, Laurie; daughters Chloe, 9, Alana and Kayla, both 7, and Ellia, 5
Hobbies: Playing piano, reading
Education: Bachelor's of science in biology, California Institute of Technology; medical school at Washington University in St. Louisl residency in ophthalmology, Barnes Hospital and Washington University Medical Center; fellowship in pediatric ophthalmology, Children's Hospital in Washington
Contact: Atlantic Eye MD, 8040 N. Wickham Road, Melbourne, 321-757-7272
Return to Top of Page
ANGIE'S LIST
January, 2012
 Dr. Frederick Ho has been awarded the prestigious 2011 Angie's List Superior Service Award, an honor bestowed
annually on appropriately 5 percent of all the businesses rated on the nation's leading provider of consumer reviews.
Dr. Frederick Ho has been awarded the prestigious 2011 Angie's List Superior Service Award, an honor bestowed
annually on appropriately 5 percent of all the businesses rated on the nation's leading provider of consumer reviews.
"Only a fraction of businesses rated on Angie's List can claim the sterling customer service record of being a Superior Service Award winner because we set a high bar," said Angie's List Founder Angie Hicks. " The fact that Frederick Ho, M.D. can claim Superior Service Award status speaks volumes about its dedication to consumers.
Thank you.
Frederick Ho, M.D.
Return to Top of Page
FLORIDA TODAY NEWSPAPER
Surgery and Laser Center Wins Accreditation.
Oct 27, 2011
Atlantic Surgery and Laser Center in Melbourne was awarded the maximum of three years of full accreditation by the Accreditation Association for Ambulatory Health Care.
The surgery center provides surgeons with the state of art technology to perform cataract surgery, multifocal lens implants, toric lens implants, glaucoma surgery, eye muscle surgery and eyelid procedures.
“Earning the longest possible term of full accreditation for a new surgery center is outstanding,” said Dr. Frederick Ho, medical director of Atlanic Eye MD and Atlantic Surgery and Laser Center, in a news releases. “I see this as a direct reflection of our dedication to excellence in ophthalmology and surgery.”
Return to Top of Page